What are the Symptoms of Cushing Syndrome?
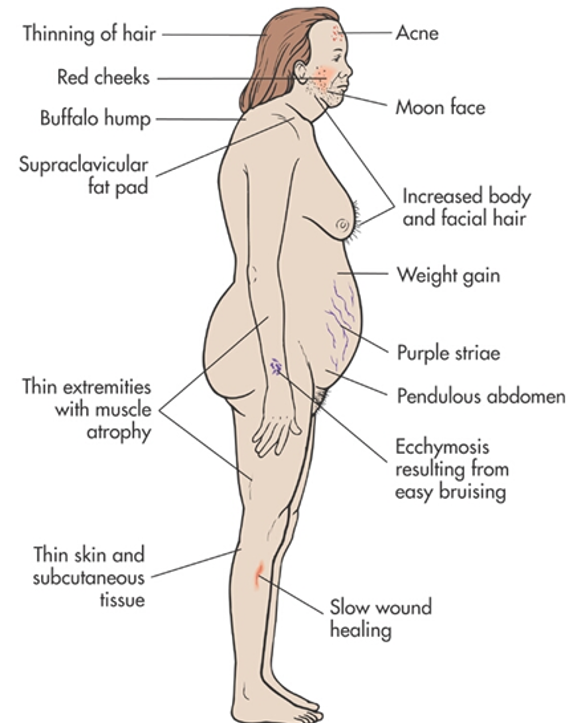
Cushing Syndrome causes many symptoms including weight gain, increased fat deposition in the face and back, easy brusing, thin skin, stretch marks on skin, acne, and depression. Symptoms of Cushing syndrome can vary widely, and some patients with cortisol overproduction can even be asymptomatic, meaning they feel “normal”; often because they have lived with the disease undiagnosed and got used to the fact that this is how life now feels like.The Most Common Symptoms of Cushing Syndrome Are:
 Cushing Syndrome causes many symptoms throughout the body.
Cushing Syndrome causes many symptoms throughout the body.
- Weight gain with central obesity (meaning unusual fat deposition around your abdomen)
- Facial rounding and plethora (called moon face)
- Supraclavicular and dorsocervical fat pads (fat deposits on the back; “buffalo hump”)
- Easy bruising, thin skin
- Poor wound healing
- Purple striae (stretch marks, especially on the lower abdomen and upper thighs)
- Proximal muscle weakness
- Emotional and neurocognitive changes (Variable, but may be: anxiety, depression, memory problems, etc)
- Opportunistic and fungal infections
- Acne
- Hirsutism (excessive facial hair)
What are the signs of Cushing syndrome your doctor can pick up on a physical exam or during laboratory tests?
- Hypertension (high blood pressure)
- Osteopenia (weak bones)
- Osteoporosis (weak bones)
- Fasting hyperglycemia (high blood sugars)
- Diabetes mellitus
- Hypokalemia (low blood potassium
- Hyperlipidemia (High blood lipids; fat)
- Leukocytosis (High white blood count)
What is Subclinical Cushing syndrome (subclinical hypercortisolism)?
Overt Cushing syndrome (meaning the signs and symptoms are so obvious that a 3rd year medical school student should be able to make the diagnosis is relatively rare, occurring in only about 10 patients per one million. However, slight overproduction of cortisol, what we call “subclinical hypercortisolism” or “subclinical Cushing syndrome” is very common. This may be related to an adrenal tumor producing too much cortisol.- Subclinical Cushing syndrome may not be as clinically insignificant as previously thought.
- The diagnosis of the syndrome is somewhat cumbersome for doctors not used to looking for it. We, at the Carling Adrenal Center, see several of these patients a week, and we can often arrive at the correct diagnosis very quickly.
- Most patients present with an “adrenal incidentaloma”; an adrenal tumor appearing on a X-ray (scan) done for other reasons. Then you need a laboratory (combination of blood and urine tests) work-up for optimal outcome
- Given the low rate of complications, we recommend minimally invasive adrenalectomy in patients with biochemically proven or suspected subclinical Cushing syndrome who are appropriate surgical candidates.