Cushing Syndrome and Cancer Risk: A Call for Awareness and Treatment

Cushing Syndrome and Cancer Risk: A Call for Awareness and Treatment
Imagine a condition that not only disrupts your body's hormonal balance but also silently increases your risk of developing cancer. This is the reality for those diagnosed with Cushing syndrome (CS), a rare but serious disorder caused by prolonged exposure to high levels of cortisol, the body's stress hormone. A groundbreaking study published in The Journal of Clinical Endocrinology & Metabolism in 2025 has shed new light on the link between CS and cancer, revealing a significantly higher cancer incidence among affected individuals. This discovery underscores the urgent need for early diagnosis, effective treatment, and specialized care, such as the advanced adrenal surgery offered at the Carling Adrenal Center. In this blog post, we'll explore the study's findings, the implications for those with CS, and why timely intervention is critical.
Understanding Cushing Syndrome
Cushing syndrome occurs when the body is exposed to excessive cortisol, often due to a tumor in the adrenal glands (adrenal CS), pituitary gland (Cushing disease), or, less commonly, ectopic sources. Cortisol plays a vital role in regulating metabolism, immune response, and stress, but too much of it can wreak havoc. Symptoms include weight gain (especially around the abdomen), a round face, thinning skin, muscle weakness, and mood changes. Beyond these visible signs, CS is associated with serious complications like obesity, diabetes, hypertension, and cardiovascular disease, all of which can significantly reduce quality of life and life expectancy.
The 2025 study, conducted in Taiwan using data from the National Health Insurance program (2006–2017), provides the first comprehensive look at CS epidemiology in an Asian population. It identified 1,278 newly diagnosed CS cases, with an incidence rate of 4.04–5.02 per million person-years, higher than previous estimates from Western countries (1.8–3.2 per million). Notably, 80% of patients were female, and the mean age at diagnosis was 45.3 years. The study also found that adrenal CS (64.6%) was more common than Cushing disease (35.4%) in Taiwan, a contrast to Western data where pituitary causes predominate.
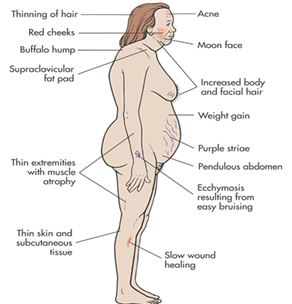
Figure 1: Cushing Syndrome causes many symptoms throughout the body, as shown above.
The Cancer Connection
The most striking finding of the study is the increased cancer risk among CS patients. Among 1,246 CS patients without prior cancer, 54 developed cancer during an average follow-up of 5.56 years, yielding an incidence rate of 7.77 per 1,000 person-years. The standardized incidence ratio (SIR) for cancer was 2.08 (95% CI 1.54–2.75), meaning CS patients had more than double the cancer risk of the general population. This risk was consistent across genders, with women (SIR 2.04) and men (SIR 2.22) both showing elevated rates.
The cancers most commonly observed were liver (27.7%), kidney (16.7%), and lung (13.0%), followed by breast, pancreas, and colon. Compared to Taiwan’s general population, where breast and colon cancers are more prevalent, CS patients showed a disproportionately high incidence of liver, kidney, and pancreatic cancers. The study suggests that prolonged hypercortisolism, which drives obesity and diabetes, may contribute to this increased risk. These conditions are known to promote cancer through mechanisms like hyperinsulinemia, systemic inflammation, and enhanced activity of insulin-like growth factor-1 (IGF-1), which can stimulate tumor growth.
Why This Matters
The link between CS and cancer is a wake-up call for patients, healthcare providers, and researchers. CS is already associated with a high mortality rate, primarily due to cardiovascular complications. The standardized mortality ratio (SMR) in the study was 1.56 (95% CI 0.94–2.43), indicating a higher risk of death compared to the general population. The addition of cancer as a significant risk further amplifies the urgency of managing CS effectively.
Obesity and diabetes, common in CS, are well-established cancer risk factors. The study notes that hypercortisolism can exacerbate these conditions, creating a perfect storm for cancer development. For example, glucocorticoids (like cortisol) may directly promote liver and pancreatic cancer progression through pathways involving endoplasmic reticulum stress and autophagy. Even after treatment, some patients continue to struggle with obesity and glucose abnormalities, suggesting that the effects of long-term cortisol exposure may persist.
The Need for Timely Treatment
The study emphasizes that early diagnosis and treatment of CS are critical to mitigating its complications, including cancer risk. Untreated CS can lead to irreversible damage, and the longer hypercortisolism persists, the greater the risk of developing obesity, diabetes, and potentially cancer. Treatment typically involves surgery to remove the tumor causing excess cortisol production, followed by medical therapy or radiation in some cases.
For adrenal CS, which was more common in the study, surgical removal of the affected adrenal gland (adrenalectomy) is often the first-line treatment. The study suggests that adrenalectomy achieves near-100% remission rates for adrenal CS, highlighting its effectiveness. However, the success of surgery depends on the expertise of the surgical team and the quality of post-operative care. This is where specialized centers like the Carling Adrenal Center stand out.
The Carling Adrenal Center: A Beacon of Hope
When it comes to adrenal surgery, the Carling Adrenal Center in Tampa, Florida, is a global leader. Founded by Dr. Tobias Carling, a world-renowned adrenal surgeon, the center specializes in minimally invasive adrenalectomy techniques that offer superior outcomes for CS patients. The center’s approach, particularly the Mini Back Scope Adrenalectomy (MBSA), is considered the gold standard for adrenal surgery.
The MBSA is a minimally invasive procedure performed through a small incision in the back, allowing for precise removal of the adrenal tumor with minimal disruption to surrounding tissues. Compared to traditional open surgery or even standard laparoscopic approaches, the MBSA offers several advantages:
- Reduced Recovery Time: Patients typically return to normal activities within days, compared to weeks for open surgery.
- Lower Complication Rates: The procedure minimizes blood loss and reduces the risk of infection or other complications.
- Improved Cosmetic Outcomes: The small incision results in minimal scarring, a significant consideration for many patients.
- High Success Rates: The Carling Adrenal Center reports exceptional remission rates for adrenal CS, aligning with the near-100% success noted in the study.
Dr. Carling’s expertise, combined with the center’s state-of-the-art facilities, ensures that patients receive personalized care tailored to their specific condition. The center also emphasizes comprehensive follow-up to monitor for recurrence and manage any residual metabolic complications, such as obesity or diabetes, which could contribute to cancer risk.
What Can Patients Do?
For individuals diagnosed with CS, the study’s findings highlight the importance of proactive management. Here are some steps to consider:
- Seek Early Diagnosis: If you experience symptoms like unexplained weight gain, fatigue, or high blood pressure, consult an endocrinologist. Early detection can prevent long-term complications.
- Choose Specialized Care: For adrenal CS, seek out centers like the Carling Adrenal Center, where expertise in minimally invasive adrenalectomy can maximize treatment success.
- Monitor Cancer Risk: After treatment, work with your healthcare team to screen for cancers, especially liver, kidney, and pancreatic, given their higher incidence in CS patients.
- Manage Metabolic Health: Address obesity and diabetes through lifestyle changes, medication, or weight loss programs to reduce cancer risk.
- Stay Informed: Understanding the risks associated with CS empowers patients to advocate for their health and seek timely interventions.
Looking Ahead
The Taiwan study is a landmark in CS research, providing the first evidence of a significant cancer risk in this population. It also fills a critical gap in understanding CS epidemiology in Asia, where adrenal CS appears more prevalent than previously thought. However, the study has limitations, such as its focus on treated CS cases and potential misclassification of CS etiology. Future research should explore the mechanisms linking hypercortisolism to cancer and investigate whether remission fully mitigates this risk.
For now, the message is clear: Cushing syndrome is not just a hormonal disorder—it’s a condition with far-reaching consequences, including a heightened cancer risk. By prioritizing early diagnosis, effective treatment, and specialized surgical care at places like the Carling Adrenal Center, patients can take control of their health and reduce the long-term impact of this challenging condition.
If you or a loved one has been diagnosed with Cushing syndrome, don’t wait. Consult a specialist, explore your treatment options, and consider the unparalleled expertise of the Carling Adrenal Center for adrenal surgery. Your health—and potentially your life—may depend on it.
Reference
- Wu WC, Wu JL, Huang TS, Li CY, Li HY. Cushing Syndrome Is Associated With a Higher Risk of Cancer-A Nationwide Cohort Study. J Clin Endocrinol Metab. 2025 Apr 22;110(5):1419-1426. PMID: 38867482.
Additional Resources:
- Learn more about the Carling Adrenal Center
- Learn more about Dr. Tobias Carling
- Learn more about our sister surgeons at the Norman Parathyroid Center, and Clayman Thyroid Center.
- Learn more about the Hospital for Endocrine Surgery