What is the Best Adrenal Operation for Cushing Syndrome Tumors?
Without a doubt, the best operation for removing the adrenal tumor that is causing Cushing Syndrome and Hypercortisolism is the Mini Back Scope Adrenalectomy (MBSA). The operation can also be called the Mini Posterior Retroperitoneoscopic Adrenalectomy, because the operation is perfomed with very small scopes that go through the lower, outer back.The Mini Back Scope Adrenalectomy (MBSA) is the preferred technique in over 95% of adrenal surgery cases, and close to 100% in patients with Cushing Syndrome and Hypercortisolism. There are many reasons this technique is preferred over any of the other techniques. The operation is performed with a scope and three small incisions at the small of the back of the patients. The cosmetic outcome is exceptional. This provides a very direct approach to the adrenal gland. The surgeons of the Carling adrenal center popularized this technique and have been using this operative approach for more than 10 years and have more experience than any other center in the United States.
How is a Mini Back Scope Adrenalectomy (MBSA) Performed? The way the operation is done, in experienced hands, leads to no blood loss. The other advantages include that it is faster with less mobilization doing the operation. All these factors lead to less pain for the patient with a shorter length of stay, faster recovery, faster return to normal activities and work. The advantage of less mobilization means that there is less risk of injury to surrounding structures such as the such as the kidney, liver, spleen, pancreas, bowel, or major vessels such as the inferior vena cava; IVC.
Dr Carling's Experience with Cushing Syndrome and Hypercortisolism. It is believed that Dr. Carling has performed more Mini Back Scope Adrenalectomy (MBSA) for adrenal tumors than any other surgeon in the United States. When performed for Cushing Syndrome and Hypercortisolism this operation typically takes Dr. Carling less than 25-35 minutes. By going through the sides of the back the surgeon has a very direct approach to the adrenal gland with the Mini Back Scope Adrenalectomy (MBSA). Dr. Carling popularized this technique while he was Chief of Endocrine Surgery at Yale University Medical School and has been using this operative approach for a decade on hundreds of patients with Cushing Syndrome and Hypercortisolism. Note, that this is a very advanced technique--surgeons that operate on adrenal glands only a few times per year are not going to offer you this operation, so be careful. If your surgeon is going to operate through the front of the abdomen to get to the adrenal gland located in the very back, then get a second opinion and find a surgeon that does lots of these--your local surgeon does not.
What are the Benefits of Surgery for Cushing Syndrome and Hypercortisolism?
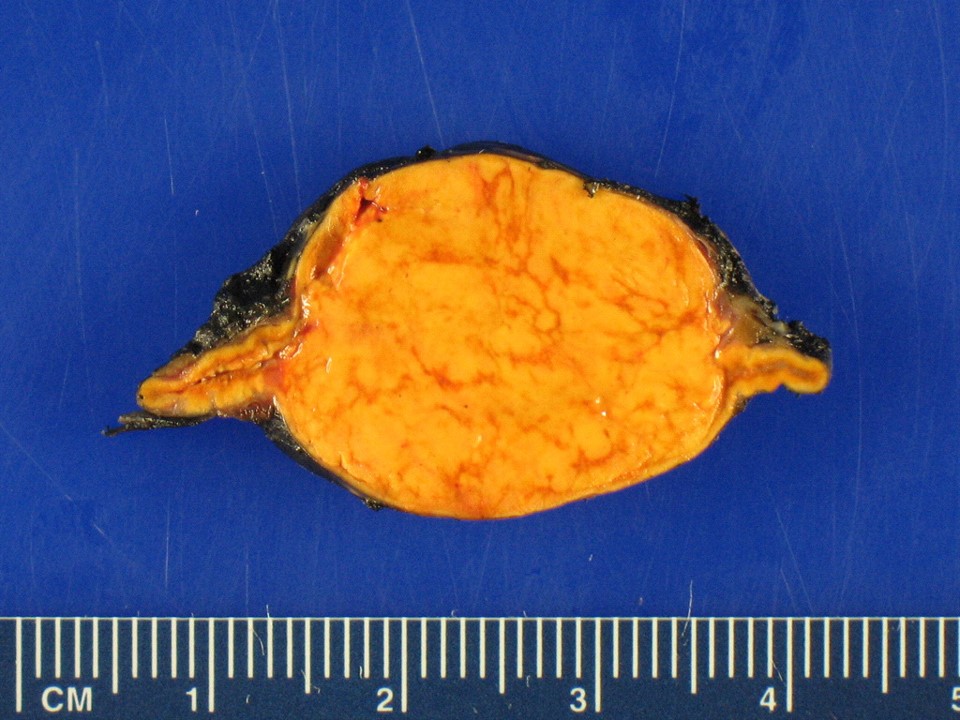 Adrenal tumor producing too much cortisol causing Cushing syndrome.
NUMEROUS! Adrenal surgery is the only curative therapy for Cushing syndrome due to adrenal tumor disease. In patients with ACTH-independent Cushing syndrome due to functional adrenal adenomas recovery after adrenalcetomy of normal function of suppressed hypothalamus, pituitary, and contralateral adrenal gland may be delayed. Therefore, the patients often require hormone replacement therapy for several weeks to months after curative adrenalectomy. This is especially important to understand, and we will work with your endocrinologist, so you have a crystal-clear plan for weaning off your hormone replacement after surgery. Recovery of HPA (Hypothalamus, Pituitary, Adrenal) axis can be evaluated by measuring serum cortisol level with blood samples obtained before the morning hydrocortisone dose, followed by an ACTH (Cosyntropin) stimulation test starting when the level is 7.4 μg/ dl (200 nmol/l) or more. The axis has recovered if the baseline or stimulated level is approximately 18 μg/dl (500 nmol/l) or greater. Patients with cortisol levels below 5 μg/dl (138 nmol/l) should remain on glucocorticoids (hydrocortisone) until retested. In the literature, patients with Cushing syndrome have a greater (more than tenfold) risk of developing venous thromboembolism (blood clots, pulmonary embolism), when undergoing surgery, and perioperative hypercoagulability prophylaxis is recommended. Again, therefore you want the most experienced, safe, and efficient surgeons doing your adrenalectomy. Also, you want a swift and efficient operation. It is not uncommon that an adrenalectomy that would take 2-4 hours at the most prestigious hospitals, can be performed by Dr. Carling in 20-30 minutes. Again, there is no value in a fast operation, per se. However, a faster operation means less time under general anesthesia. Although, general anesthesia is very safe, the longer time the patient is under general anesthesia, the greater risk of anesthesia-related complications such as nausea, vomiting, neurocognitive symptoms, blood clots, pulmonary embolism, urinary retention (emptying the bladder), infections and in some cases long-term effects on cognition and memory. Adrenalectomy in Cushing syndrome leads to improvement in hypertension, diabetes, obesity, and dyslipidemia (poor blood fat levels), and glucose metabolism. Importantly, adrenal surgery has been demonstrated to decrease the cardiovascular risk factors. Furthermore, we see improvement in muscle weakness, bone density (reversal of osteoporosis), diabetes, bruising, wound healing, emotional and neurocognitive functions, acne, and hirsutism (excessive facial hair) Within 6-12 months, many patients who have had surgery for Cushing syndrome describe themselves as a new person. Occasionally, some doctors wish to treat patients with medications (e.g. Korlym) instead of adrenal surgery. This is a mistake. Adrenal surgery is vastly superior, much more effective, and less expensive than Korlym medication. Korlym should be used in preparation for surgery or reserved for the rare patients were adrenal surgery is not possible.
Adrenal tumor producing too much cortisol causing Cushing syndrome.
NUMEROUS! Adrenal surgery is the only curative therapy for Cushing syndrome due to adrenal tumor disease. In patients with ACTH-independent Cushing syndrome due to functional adrenal adenomas recovery after adrenalcetomy of normal function of suppressed hypothalamus, pituitary, and contralateral adrenal gland may be delayed. Therefore, the patients often require hormone replacement therapy for several weeks to months after curative adrenalectomy. This is especially important to understand, and we will work with your endocrinologist, so you have a crystal-clear plan for weaning off your hormone replacement after surgery. Recovery of HPA (Hypothalamus, Pituitary, Adrenal) axis can be evaluated by measuring serum cortisol level with blood samples obtained before the morning hydrocortisone dose, followed by an ACTH (Cosyntropin) stimulation test starting when the level is 7.4 μg/ dl (200 nmol/l) or more. The axis has recovered if the baseline or stimulated level is approximately 18 μg/dl (500 nmol/l) or greater. Patients with cortisol levels below 5 μg/dl (138 nmol/l) should remain on glucocorticoids (hydrocortisone) until retested. In the literature, patients with Cushing syndrome have a greater (more than tenfold) risk of developing venous thromboembolism (blood clots, pulmonary embolism), when undergoing surgery, and perioperative hypercoagulability prophylaxis is recommended. Again, therefore you want the most experienced, safe, and efficient surgeons doing your adrenalectomy. Also, you want a swift and efficient operation. It is not uncommon that an adrenalectomy that would take 2-4 hours at the most prestigious hospitals, can be performed by Dr. Carling in 20-30 minutes. Again, there is no value in a fast operation, per se. However, a faster operation means less time under general anesthesia. Although, general anesthesia is very safe, the longer time the patient is under general anesthesia, the greater risk of anesthesia-related complications such as nausea, vomiting, neurocognitive symptoms, blood clots, pulmonary embolism, urinary retention (emptying the bladder), infections and in some cases long-term effects on cognition and memory. Adrenalectomy in Cushing syndrome leads to improvement in hypertension, diabetes, obesity, and dyslipidemia (poor blood fat levels), and glucose metabolism. Importantly, adrenal surgery has been demonstrated to decrease the cardiovascular risk factors. Furthermore, we see improvement in muscle weakness, bone density (reversal of osteoporosis), diabetes, bruising, wound healing, emotional and neurocognitive functions, acne, and hirsutism (excessive facial hair) Within 6-12 months, many patients who have had surgery for Cushing syndrome describe themselves as a new person. Occasionally, some doctors wish to treat patients with medications (e.g. Korlym) instead of adrenal surgery. This is a mistake. Adrenal surgery is vastly superior, much more effective, and less expensive than Korlym medication. Korlym should be used in preparation for surgery or reserved for the rare patients were adrenal surgery is not possible.
What is the treatment for ACTH-Independent Bilateral Adrenal Disease?
The less common causes of ACTH-independent Cushing syndrome that are the familial and sporadic forms of bilateral macronodular (BAIMAH) and micronodular adrenal hyperplasia with its pigmented variant are also referred to as primary pigmented nodular adrenocortical disease (PPNAD). Adrenalectomy is the only potentially curative treatment. The Mini-Back Scope Adrenalectomy (MBSA) is the preferred technique in >95 % of adrenal surgery cases for both uni- and bilateral Adrenal (ACTH-independent) Cushing syndrome. This is especially important to know for some candidates with less common causes of ACTH-independent Cushing syndrome that are the familial and sporadic forms of bilateral macronodular (BAIMAH) and micronodular adrenal hyperplasia with its pigmented variant also referred to as primary pigmented nodular adrenocortical disease (PPNAD). Patients with BAIMAH and PPNAD can be excellent candidates for partial (cortex-sparing) adrenalectomy and should have their operations performed at the highest-volume adrenal surgery center, as possible. A complete bilateral adrenalectomy sometimes (but rarely) may have to be performed and will inevitably cause permanent adrenal insufficiency requiring a lifelong mineralocorticoid and glucocorticoid replacement therapy. These patients require special attention and must have a booked follow up appointment with their endocrinologist before surgery. Patients and their family members need to know about adrenal insufficiency signs and symptoms including instructions on “sick day” dose adjustment and when and how to use emergency hydrocortisone injection. Patients should be provided with medical alert bracelets and hydrocortisone sodium succinate vials for emergency use. This is particularly important to understand, and we will work with your endocrinologist, so this is addressed prior to surgery. Occasionally, some doctors wish to treat patients with medications (e.g. Korlym) instead of adrenal surgery. This is a mistake. Adrenal surgery is vastly superior, much more effective, and less expensive than Korlym medication. Korlym should be used in preparation for surgery or reserved for the rare patients were adrenal surgery is not possible
What is the treatment for “failed” pituitary treatment of Cushing Disease?
Cushing disease (CD) is the consequence of chronic exposure to glucocorticoids due to a pituitary adenoma secreting ACTH. It comprises a large spectrum of signs and symptoms that cause an increased morbidity and mortality, and deterioration in quality of life (QoL). The first-line treatment option is surgical resection of the pituitary adenoma. However, 31% of patients with Cushing disease will require a secondary treatment option, either due to a failure by a first pituitary surgery to control the symptoms or due to recurrence of cortisol hypersecretion. Remember, too much cortisol is very toxic to the body. This is a big problem. Thus, the second-line treatment options sometimes must be complete bilateral adrenalectomy. The goal is to remove any cells in the body that can overproduce the toxic cortisol. Recent studies have shown that bilateral adrenalectomy is an increasingly used and essential treatment option when re-operative pituitary surgery is no longer an option. Compared to other options such as adrenal gland radiation or medical treatment (e.g. Korlym), bilateral adrenalectomy lowers morbidity and mortality rates, as well as improves quality-of-life. The Mini-Back Scope Adrenalectomy (MBSA) is the preferred technique in “failed” Cushing Disease. A complete bilateral adrenalectomy sometimes (but rarely) may have to be performed and will inevitably cause permanent adrenal insufficiency requiring a lifelong mineralocorticoid and glucocorticoid replacement therapy. These patients require special attention and must have a booked follow up appointment with their endocrinologist before surgery. Patients and their family members need to know about adrenal insufficiency signs and symptoms including instructions on “sick day” dose adjustment and when and how to use emergency hydrocortisone injection. Patients should be provided with medical alert bracelets and hydrocortisone sodium succinate vials for emergency use. This is particularly important to understand, and we will work with your endocrinologist, so this is addressed prior to surgery. Occasionally, some doctors wish to treat patients with medications (e.g. Korlym) instead of adrenal surgery. This is a mistake. Adrenal surgery is vastly superior, much more effective, and less expensive than Korlym medication. Korlym should be used in preparation for surgery or reserved for the rare patients were adrenal surgery is not possible.Become Our Patient
Patients needing adrenal surgery travel from all over the world to have adrenal surgery with Dr. Carling, the most experienced adrenal surgeon. This page discusses how you can have your adrenal operation at the Carling Adrenal Center with Dr. Carling himself.What to read next
- Mini-Back-Scope-Surgery - the preferred adrenal operation for 95% of adrenal tumors.
- More about our founder Dr. Tobias Carling - the most experienced adrenal surgeon in the world.
- How to become our patient, and have Dr. Carling perform your adrenal surgery.
- The 8 ways adrenal surgery can be performed - learn about the different types of surgery and when they are appropriate.