Why Do You Need to Take Conn's Syndrome Seriously?
Because too much aldosterone is very toxic. Too high aldosterone levels lead to toxic effects called
Target Organ Damage). Furthermore, we are passionate to educate patinets and doctors because today only a fraction of all patients (< 5%) are being diagnosed, and an even smaller fraction are being offered curative surgery. This toxic (and very silent) disease can often be cured by a 20-30-minute
Mini-Back Scope Adrenalectomy (MBSA) operation. Primary aldosteronism is important not only because of its high prevalence (very common disease), but also because patients with primary aldosteronism have a very high cardiovascular morbidity and mortality. It is
very silent and deadly. The risk of stroke, heart attack and heart arrhythmias are increased 10-fold; 1,000%) compared to age-, sex- and blood pressure matched patients with essential hypertension (high blood pressure NOT related to an adrenal tumor).
Why is primary aldosteronism so important, and why are we so eager to get patients treated? Treating primary hyperaldosteronism by surgery
Mini-Back Scope Adrenalectomy (MBSA) cures hypokalemia, lowers blood pressure, reduces the number of antihypertensive medications required, and improves parameters of impaired cardiac and renal function. Even if you decide surgery is not for you (maybe you are at a very advanced age, and have multiple comorbidities, and your heart is not strong enough for a 30-minute procedure), we want you to be diagnosed accurately because there are some medications (albeit not as good or cost-effective as surgery) that may be beneficial to you. These include mineralcorticoid receptor antagonists.
What is the Role of Too Much Aldosterone in Target Organ Damage?
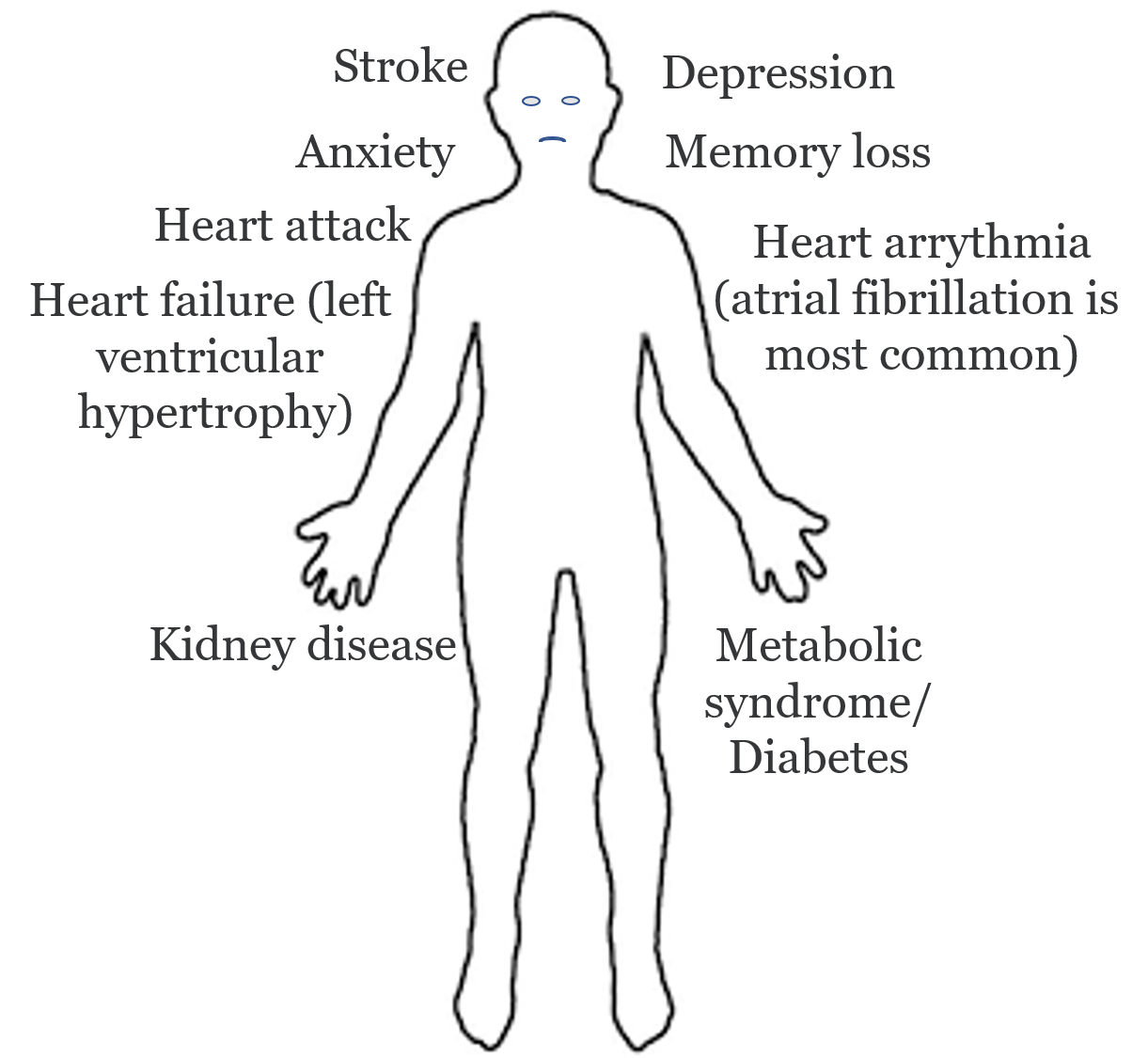 Complications of primary hyperaldosteronism (Conn’s syndrome): The consequences of undiagnosed and untreated Conn’s syndrome.
Remember, too much aldosterone (often from a bad aldosterone-producing adrenal adenoma) is toxic to your body. This toxicity is called Target Organ Damage. Traditionally, aldosterone has been considered the main regulator of water and electrolyte homeostasis due to its effects on epithelial cells, particularly in the collecting ducts of the kidney and distal colon. The physiological actions of aldosterone in other tissues were much less evident, but over the last 15 years, studies both in humans and animal models have gained new insights on its effects, that are mainly targeted in the heart, blood vessels, kidney, and central nervous system (CNS). Please note that the below discussion is technical and reviews some of the latest science on primary hyperaldosteronism.
Complications of primary hyperaldosteronism (Conn’s syndrome): The consequences of undiagnosed and untreated Conn’s syndrome.
Remember, too much aldosterone (often from a bad aldosterone-producing adrenal adenoma) is toxic to your body. This toxicity is called Target Organ Damage. Traditionally, aldosterone has been considered the main regulator of water and electrolyte homeostasis due to its effects on epithelial cells, particularly in the collecting ducts of the kidney and distal colon. The physiological actions of aldosterone in other tissues were much less evident, but over the last 15 years, studies both in humans and animal models have gained new insights on its effects, that are mainly targeted in the heart, blood vessels, kidney, and central nervous system (CNS). Please note that the below discussion is technical and reviews some of the latest science on primary hyperaldosteronism.
Damage to your heart
The main pathological effects of aldosterone excess on the heart are vascular and perivascular inflammation, fibrosis, and myocardial hypertrophy. A direct role of aldosterone in myocardial inflammatory damage was demonstrated in transgenic rats overexpressing the human renin and angiotensinogen genes: hypersecretion of aldosterone promoted hypertrophy, cardiac remodeling and fibrosis, independent of blood pressure (this is BAD for your heart). Studies in patients suggest that primary hyperaldosteronism is associated with increased prevalence and severity of left ventricular hypertrophy (this is when your heart grows too big and does not function properly; not good). The aldosterone effect by itself, regardless of the level of blood pressure abnormality demonstrated that primary hyperaldosteronism patients have significantly higher severity of abnormal heart growth even after correction for age, gender, duration, and severity of hypertension compared to essential hypertensives (These are patients with high blood pressure but no bad adrenal tumor overproducing aldosterone).
Damage to your blood vessels
 Too much aldosterone is toxic to the inner lining of blood vessels called the endothelium, leading to increased risk of stroke, heart attack, arrhythmia, kidney failure, and premature death.
Vascular and perivascular inflammation via by too much aldosterone in myocardium (heart muscle cells) can also be observed in other vascular areas, with similar mechanisms of endothelial activation, leukocyte accumulation, and pro-fibrogenic cytokine production (this is bad inflammation in your vessels; the arteries, and veins responsible for transporting blood throughout your body). Aldosterone cause problems with relaxation of your vessels due to effect of the inner lining of vessel (this is called endothelial dysfunction). Also, aldosterone causes increased vascular stiffness. In patients with primary hyperaldosteronism, research has proven that blood vessels have a higher level of fibrosis (scar formation) in the walls of small resistance arteries.
Too much aldosterone is toxic to the inner lining of blood vessels called the endothelium, leading to increased risk of stroke, heart attack, arrhythmia, kidney failure, and premature death.
Vascular and perivascular inflammation via by too much aldosterone in myocardium (heart muscle cells) can also be observed in other vascular areas, with similar mechanisms of endothelial activation, leukocyte accumulation, and pro-fibrogenic cytokine production (this is bad inflammation in your vessels; the arteries, and veins responsible for transporting blood throughout your body). Aldosterone cause problems with relaxation of your vessels due to effect of the inner lining of vessel (this is called endothelial dysfunction). Also, aldosterone causes increased vascular stiffness. In patients with primary hyperaldosteronism, research has proven that blood vessels have a higher level of fibrosis (scar formation) in the walls of small resistance arteries.
Damage to your kidneys
Too much aldosterone is very bad for your kidneys. In fact, many of our patients with primary hyperaldosteronism already have damage to their kidneys (increased creatinine and reduced glomerular filtration rate; GFR) even before they are referred to us. Many studies with animal models of aldosterone excess have shown the involvement of aldosterone in the pathogenesis of kidney disease. The good news is that adrenalectomy (read about
Mini-Back Scope Adrenalectomy ) has proven effective in preventing further deterioration of kidney function in patients with primary hyperaldosteronism, regardless of how high their blood pressure is. No one wants to end up being dependent on a dialysis machine, so if you have high blood pressure, and slightly worsening kidney function, you need to make sure you do not have an aldosterone-producing tumor slowly killing your kidneys.
Damage to your brain (CNS; Central Nervous System)
The brain (CNS) is considered one of the main targets of aldosterone. Raised aldosterone levels in the CNS can increase blood pressure. The main consequence of aldosterone excess on the CNS is the predisposition to acute cerebrovascular events (stroke, etc), related to vascular damage that aldosterone may induce in the CNS vascular bed. To prevent future devastating injuries to your brain, patients with primary hyperaldosteronism should be treated correctly, often by surgery. Learn more about
Mini-Back Scope Adrenalectomy (MBSA).
Damage to your Quality of Life (QoL)
Quality of life (QoL) studies aim to figure out how a we feel and how our brains work, and often how a disease affects our QoL. Primary hyperaldosteronism (PA or “ALDO”) has been shown in many studies to lead to reduced quality of life. The good news is that it is reversible. This means you can feel better after curative adrenalectomy.
Not only does adrenalectomy lead to substantial improvement of the QoL of patients with PA but also restores the QoL to the level of the general population. This means that you are likely to get back to a baseline after curative surgery.
The reason the QoL is reduced tends to be related to anxiety, depressive symptoms, psychological distress, fatigue, lack of energy, reduced activity level, various emotional problems, body pain and aches, etc. The reduced quality of life tends to be especially pronounced in younger often female patients
Become Our Patient
Patients needing adrenal surgery travel from all over the world to have adrenal surgery with Dr. Carling, the most experienced adrenal surgeon. This page discusses how you can have your adrenal operation at the Carling Adrenal Center with Dr. Carling himself.
Become Our Patient Here
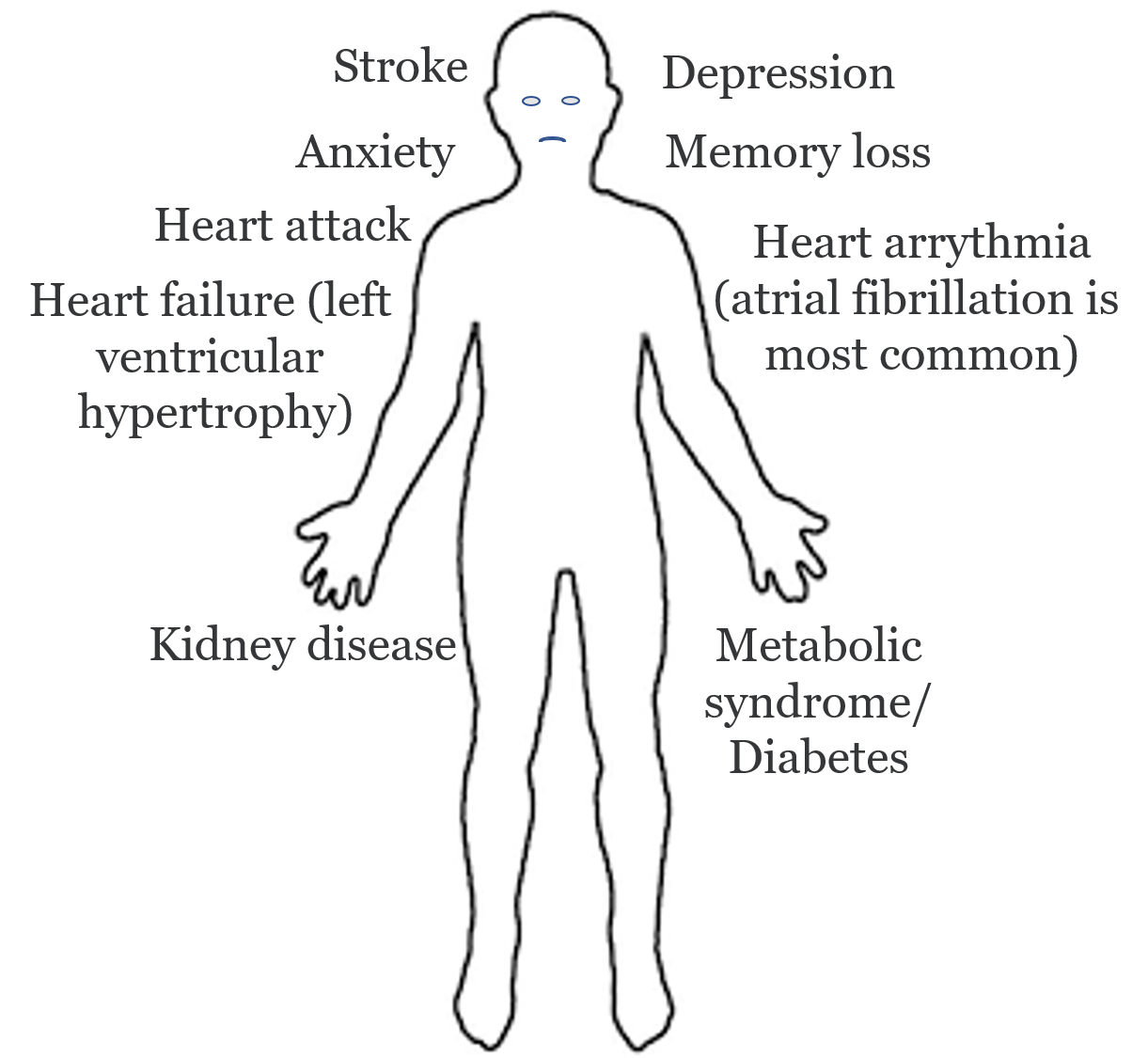 Complications of primary hyperaldosteronism (Conn’s syndrome): The consequences of undiagnosed and untreated Conn’s syndrome.
Remember, too much aldosterone (often from a bad aldosterone-producing adrenal adenoma) is toxic to your body. This toxicity is called Target Organ Damage. Traditionally, aldosterone has been considered the main regulator of water and electrolyte homeostasis due to its effects on epithelial cells, particularly in the collecting ducts of the kidney and distal colon. The physiological actions of aldosterone in other tissues were much less evident, but over the last 15 years, studies both in humans and animal models have gained new insights on its effects, that are mainly targeted in the heart, blood vessels, kidney, and central nervous system (CNS). Please note that the below discussion is technical and reviews some of the latest science on primary hyperaldosteronism.
Complications of primary hyperaldosteronism (Conn’s syndrome): The consequences of undiagnosed and untreated Conn’s syndrome.
Remember, too much aldosterone (often from a bad aldosterone-producing adrenal adenoma) is toxic to your body. This toxicity is called Target Organ Damage. Traditionally, aldosterone has been considered the main regulator of water and electrolyte homeostasis due to its effects on epithelial cells, particularly in the collecting ducts of the kidney and distal colon. The physiological actions of aldosterone in other tissues were much less evident, but over the last 15 years, studies both in humans and animal models have gained new insights on its effects, that are mainly targeted in the heart, blood vessels, kidney, and central nervous system (CNS). Please note that the below discussion is technical and reviews some of the latest science on primary hyperaldosteronism.
 Too much aldosterone is toxic to the inner lining of blood vessels called the endothelium, leading to increased risk of stroke, heart attack, arrhythmia, kidney failure, and premature death.
Vascular and perivascular inflammation via by too much aldosterone in myocardium (heart muscle cells) can also be observed in other vascular areas, with similar mechanisms of endothelial activation, leukocyte accumulation, and pro-fibrogenic cytokine production (this is bad inflammation in your vessels; the arteries, and veins responsible for transporting blood throughout your body). Aldosterone cause problems with relaxation of your vessels due to effect of the inner lining of vessel (this is called endothelial dysfunction). Also, aldosterone causes increased vascular stiffness. In patients with primary hyperaldosteronism, research has proven that blood vessels have a higher level of fibrosis (scar formation) in the walls of small resistance arteries.
Too much aldosterone is toxic to the inner lining of blood vessels called the endothelium, leading to increased risk of stroke, heart attack, arrhythmia, kidney failure, and premature death.
Vascular and perivascular inflammation via by too much aldosterone in myocardium (heart muscle cells) can also be observed in other vascular areas, with similar mechanisms of endothelial activation, leukocyte accumulation, and pro-fibrogenic cytokine production (this is bad inflammation in your vessels; the arteries, and veins responsible for transporting blood throughout your body). Aldosterone cause problems with relaxation of your vessels due to effect of the inner lining of vessel (this is called endothelial dysfunction). Also, aldosterone causes increased vascular stiffness. In patients with primary hyperaldosteronism, research has proven that blood vessels have a higher level of fibrosis (scar formation) in the walls of small resistance arteries.