Surgery for Pheochromocytoma. The Best Surgical Options for Removal of Pheochromocytomas.
The best adrenal operation for roughly 95% of pheochromocytomas (and thus, likely your pheochromocytoma) is the posterior retroperitoneal adrenalectomy, or more simply put, the Mini-Back Scope Adrenalectomy (MBSA).
Surgery for Pheochromocytoma
In general, the best adrenal operation depends on the problem that needs to be fixed. There are several factors that an expert adrenal surgeon will consider in determining which is the best adrenal operation for your pheochromocytoma:
- The size of the tumor (as measured on preoperative X-ray: oftentimes a CT scan, MRI, or specialized nuclear medicine scan)
- The type of adrenal tumor (Is it very large? Is it producing too much hormone? Does it look cancerous, or has a known cancer elsewhere in the body spread to the adrenal gland?)
- The appearance of the tumor on preoperative X-ray (Is the tumor involving surrounding structures, such as organs or vessels?)
- A history of previous abdominal operations
- The surgeon's experience with the different adrenal operations
Remember that the average number of adrenal operations by American adrenal surgeons is one per year! That means it is unlikely that your surgeons have experience with surgery for pheochromocytoma and paraganglioma. The best option is almost always to travel to the most experienced surgeon and center for your pheochromocytoma surgery.
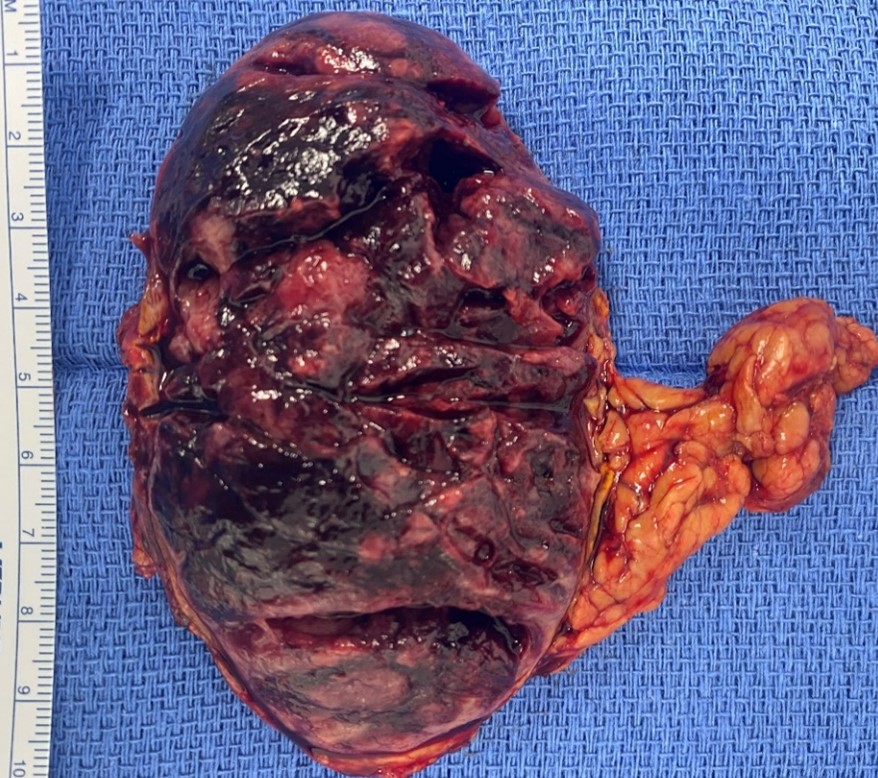 Typical right pheochromocytoma after it was removed by the Mini Back Scope Adrenalectomy (MBSA) surgery by Dr. Carling. Although the tumor was large and produced massive amounts of adrenaline-type hormones, the operation took only 23 minutes. The tumor is dark. Pheo = dark (ancient greek), chromo = color
Typical right pheochromocytoma after it was removed by the Mini Back Scope Adrenalectomy (MBSA) surgery by Dr. Carling. Although the tumor was large and produced massive amounts of adrenaline-type hormones, the operation took only 23 minutes. The tumor is dark. Pheo = dark (ancient greek), chromo = color
The Mini Back Scope Adrenalectomy (MBSA) the best adrenal operation for 95% of pheochromocytomas
Since the adrenal glands live in the back part of your abdomen, sitting on top of the kidneys (as seen in the diagram below), getting to them through the back with small scopes makes the most sense, has many tremendous benefits, and is the best adrenal operation.
Read more about the advantages of the Mini-Back-Scope Adrenal Operation.
With the way the Mini Back Scope Adrenalectomy (MBSA) operation is done, particularly when performed by an expert adrenal surgeon, there is near-zero blood loss. By going through the back, the scopes are placed directly into the space where the adrenal glands are located, and thus, less mobilization (i.e., dissection of surrounding structures). Less dissection = less blood loss AND less risk of injury to surrounding structures (such as the kidney, liver, spleen, pancreas, and bowel) or major vessels (such as the inferior vena cava). Furthermore, less dissection leads to less postoperative adhesions (scar tissue). You want the safest AND best adrenal operation for your pheochromocytoma.
The Mini Back Scope Adrenalectomy (MBSA) is the best adrenal operation. It is much faster than any other technique, since again, the scopes are placed directly into the space where the adrenal glands are, requiring less dissection. This is extremely important in every surgery, but in particular, an adrenal operation for pheochromocytoma. A fast operation means that your surgeon is skilled and efficient with an excellent team in-place to best care for you. A faster operation means less time under general anesthesia, less opportunity for blood pressure and heart rate fluctuations, which can be extreme during an adrenal operation for pheochromocytoma. Even though general anesthesia is very safe, the longer duration of time that you are under anesthesia, the greater the risk of anesthesia-related complications such as nausea, vomiting, blood clots, pulmonary embolism (blood clots to the lungs), headache, and in some cases, long-term effects on cognition and memory. As you can see, faster is better when it comes to operative time under anesthesia, and the Mini Back Scope Adrenalectomy (MBSA) is the best adrenal operation, allowing for less time (and less opportunity for adrenaline surges and blood pressure changes) on the operating room table.
 Dr. Carling and his team are focusing during a Mini Back Scope Adrenalectomy (MBSA) for pheochromocytoma.
Dr. Carling and his team are focusing during a Mini Back Scope Adrenalectomy (MBSA) for pheochromocytoma.
When performing Mini Back Scope Adrenalectomy (MBSA) for pheochromocytoma, the surgeon does not need to enter the belly. This is clearly the best adrenal operation for those with previous abdominal operations, since the surgeon does not need to encounter and contend with adhesions (scar tissue). Intra-abdominal adhesions may result from any previous belly operation such as bariatric surgery (gastric band, sleeve gastrectomy, gastric bypass), gallbladder surgery (cholecystectomy), liver surgery, stomach surgery, bowel surgery of any kind (colectomy, appendectomy, etc.), trauma surgery, or any gynecological operation (C-section, hysterectomy, etc.). By approaching your pheochromocytoma through the back, this is the best-case scenario, your surgeon will not encounter the bowel, and thus, you are not at risk of developing future intra-abdominal scars. Scarring near the bowel, or intestine, can lead to problems with small bowel obstruction, a common postoperative complication that can occur at any time after the belly surgeries listed above.
The Mini Back Scope Adrenalectomy (MBSA) is clearly the best adrenal operation for pheochromocytoma, affording many advantages over the other soon-to-be mentioned approaches. Since the Mini Back Scope Adrenalectomy (MBSA) operation has less dissection, causing less scar tissue, with quicker operating times, there is less postoperative pain and quicker recovery. Many will only require Tylenol (acetaminophen) or Motrin (ibuprofen), after the operation. Very few patients need strong painkillers, which have their own negative side effects.
The best adrenal operation for pheochromocytoma allows you to spend less than 23 hours in the hospital. Most people return to work within a few days. You can start your hobbies and exercises typically within the week following Mini Back Scope Adrenalectomy (MBSA). The cosmetic outcome is the best, far superior to any other technique, three small incisions, each less than a thumbnail length.
For patients requiring a bilateral adrenalectomy, the Mini Back Scope Adrenalectomy (MBSA) is hands-down the best adrenal operation, since there is no moving, flipping, and turning the patient around during the operation to access the adrenal glands. This is better for the patient and the entire operating room staff.
There is no question that the Mini Back Scope Adrenalectomy (MBSA). is the best adrenal operation for about 95% of all patients requiring pheochromocytoma removal. In the rare (5%) instance that the pheochromocytoma is cancerous or extremely large, typically 8-10 cm or greater, one of the other adrenal operations mentioned below is likely a better option. However, if your surgeon is not at least discussing the BEST adrenal operation with you (MBSA), then you may want to consult with a different surgeon. Adrenal surgery is almost NEVER an emergency. The tumor that needs to be removed has typically been present for at least 4-5 years, so you have time to seek an expert surgical opinion.
For the 5% of you whose tumor size or characteristics do not allow for the best adrenal operation, there are still options available. However, you must be prepared for more pain after the operation, intra-abdominal scar tissue near the intestines, longer hospital stays and recovery times, as well as a slower return to work and your normal activities and exercise. None of this sounds as fun as what can be expected after the best adrenal operation for pheochromocytoma, MBSA; however, some pheochromocytomas will not allow for the best operation.
The honorable mention approaches to pheochromocytoma are as follows:
Laparoscopic trans-abdominal, laparoscopic hand-port assisted trans-abdominal, and the standard open, along with other outdated modifications to these traditional approaches.
Read about the different approaches to adrenal surgery. Remember, not all “minimally-invasive” adrenal operations for pheochromocytoma are created equally. Learn the Top 5 Reasons Laparoscopic Adrenalectomy Should Be Avoided.
Adrenal surgery can be performed different ways, but the best adrenal operation for almost all pheochromocytomas is the Mini Back Scope Adrenalectomy (MBSA). Your adrenal operation for pheochromocytoma should be dictated by your specific circumstances, since one operation does not fit all tumors. If your surgeon is not comfortable with all different techniques offered by expert surgeons, including MBSA, then you should consider a second opinion. A customized, individual approach to your pheochromocytoma will result in the best possible outcome.
Laparoscopic Hand-port Assisted Trans-Abdominal Adrenalectomy is used for the 5% of pheochromocytoma tumors that are huge
This approach is a hybrid between laparoscopic transabdominal adrenalectomy (LTA) and Open Standard Trans-Abdominal Adrenalectomy. The positioning of the patient, and approach is similar as the laparoscopic transabdominal adrenalectomy (LTA). This approach is for larger tumors (> 8-12 cm) and tumors which are suspected or known to be malignant or very large, aggressive pheochromocytomas. Also, this approach may be used dependent on the patient’s body habitus (especially obesity).
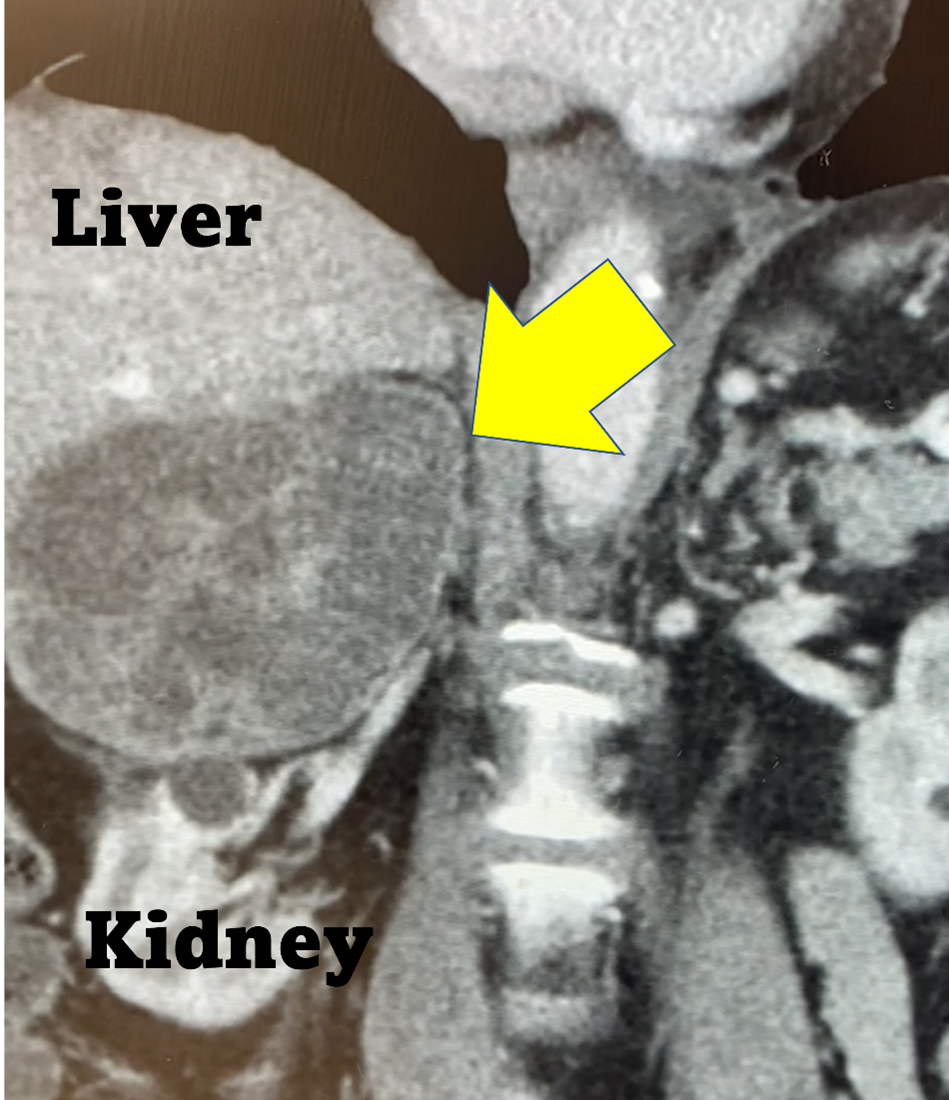 Huge 15 cm right pheochromocytoma on a CT scan. This pheochromocytoma is better removed using the Laparoscopic Hand-port Assisted Trans-Abdominal Adrenalectomy.
Huge 15 cm right pheochromocytoma on a CT scan. This pheochromocytoma is better removed using the Laparoscopic Hand-port Assisted Trans-Abdominal Adrenalectomy.
Pheochromocytoma is sometimes associated with a specific type of thyroid cancer and parathyroid tumor(s).
Learn more about thyroid disease, thyroid cancer and thyroid surgery.
Learn more about parathyroid disease and parathyroid surgery.