Interesting Adrenal Cases
Interesting case of the week: Conn' syndrome in patient where MRI missed the tumor
IToday's patient is a 54-year-old woman. She had many symptoms including high blood pressure (on 3 medications), muscle cramping, difficulty concentrating, difficulty with memory, irritability, low potassium and more.
She had already had stroke symptoms, and her kidney disease had peaked to stage 3. This is all from the toxic effects of aldosterone.
She had an MRI which was read as completely normal. She underwent adrenal vein sampling with Dr. Patel here with us at South Tampa. Dr. Patel now performs more adrenal vein sampling procedures than any interventional radiologist in the country.
You already know that adrenal vein sampling (a procedure to measure aldosterone production from each adrenal gland) has many drawbacks, and in many cases delays curative adrenal surgery.
However, this case is an exception where adrenal vein sampling was very helpful. It demonstrated that the LEFT adrenal gland tumor was the culprit. The LEFT aldosterone-producing tumor was secreting more than10 times as much aldosterone (what we called the lateralization index).
The patient had a swift 18-minute left mini back scope adrenalectomy (MBSA).
The patient did very well! She is already cured from her Conn’s syndrome and this will prevent further damage to the brain and kidneys.
Interesting case of the week: Subclinical Cushing's syndrome in Massachusetts lady
Today's patient is a 35-year-old patient from Massachusetts (although originally, she is from Berlin, Germany).
This patients’ symptoms included difficulty concentrating, facial rounding and plethora (called moon face), supraclavicular and dorsocervical fat pads, stretch marks, especially on the lower abdomen and upper thighs, weight gain with central obesity.
Her laboratory tests showed that her ACTH level was on the low side, and her low dose dexamethasone suppression test (LDDST) was borderline. This proves that her subclinical Cushing’s syndrome arose from an adrenal source (as opposed to the pituitary; Cushing’s disease).
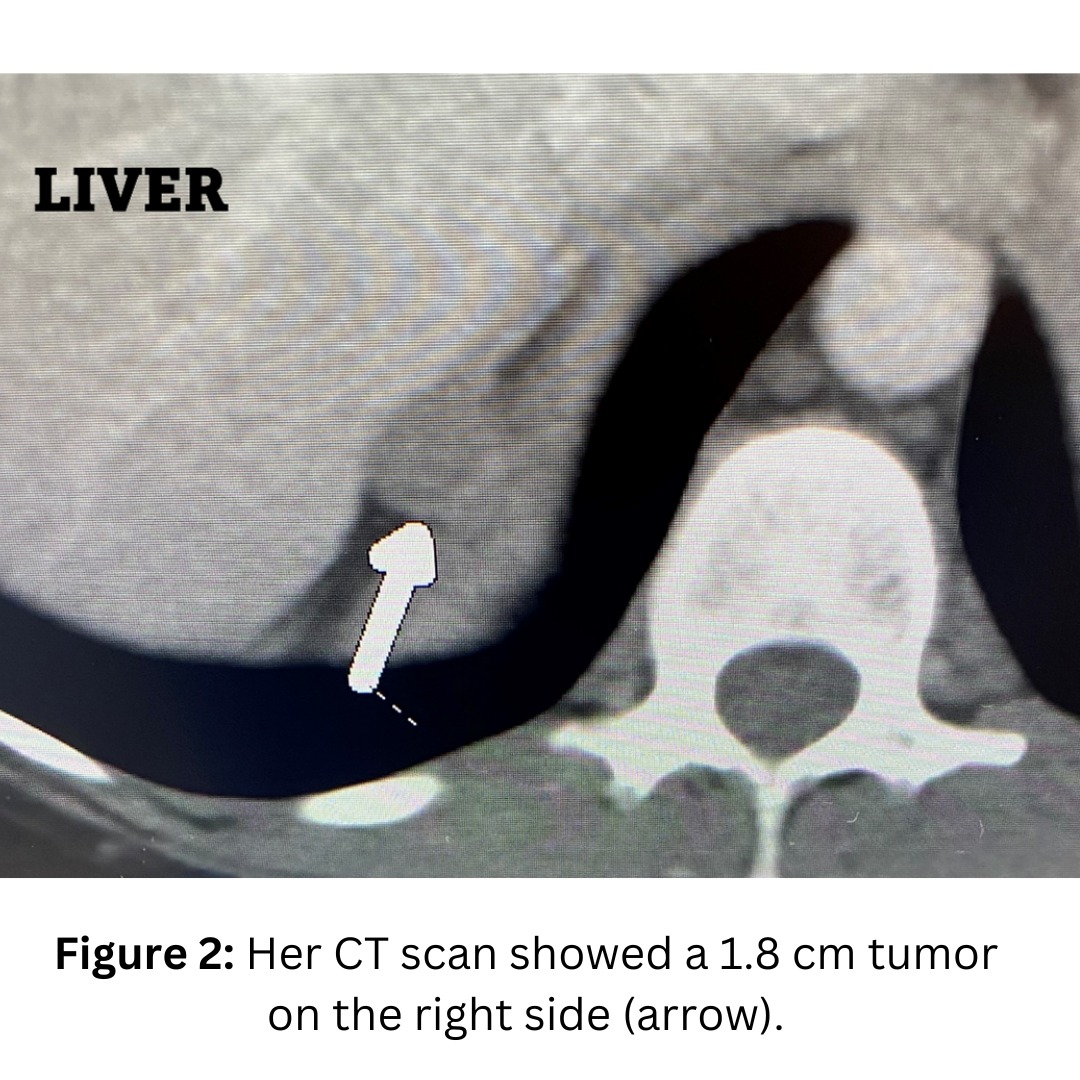
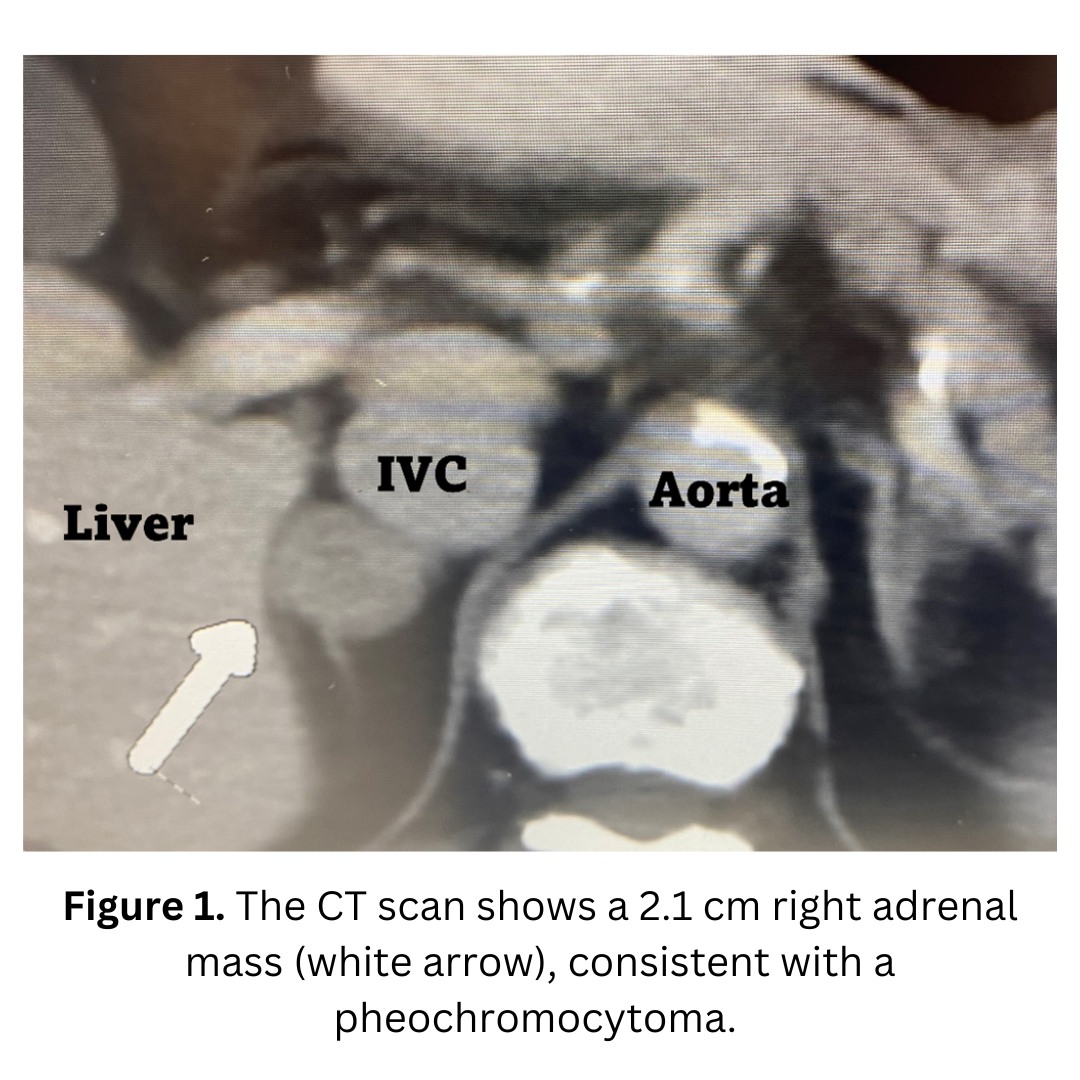
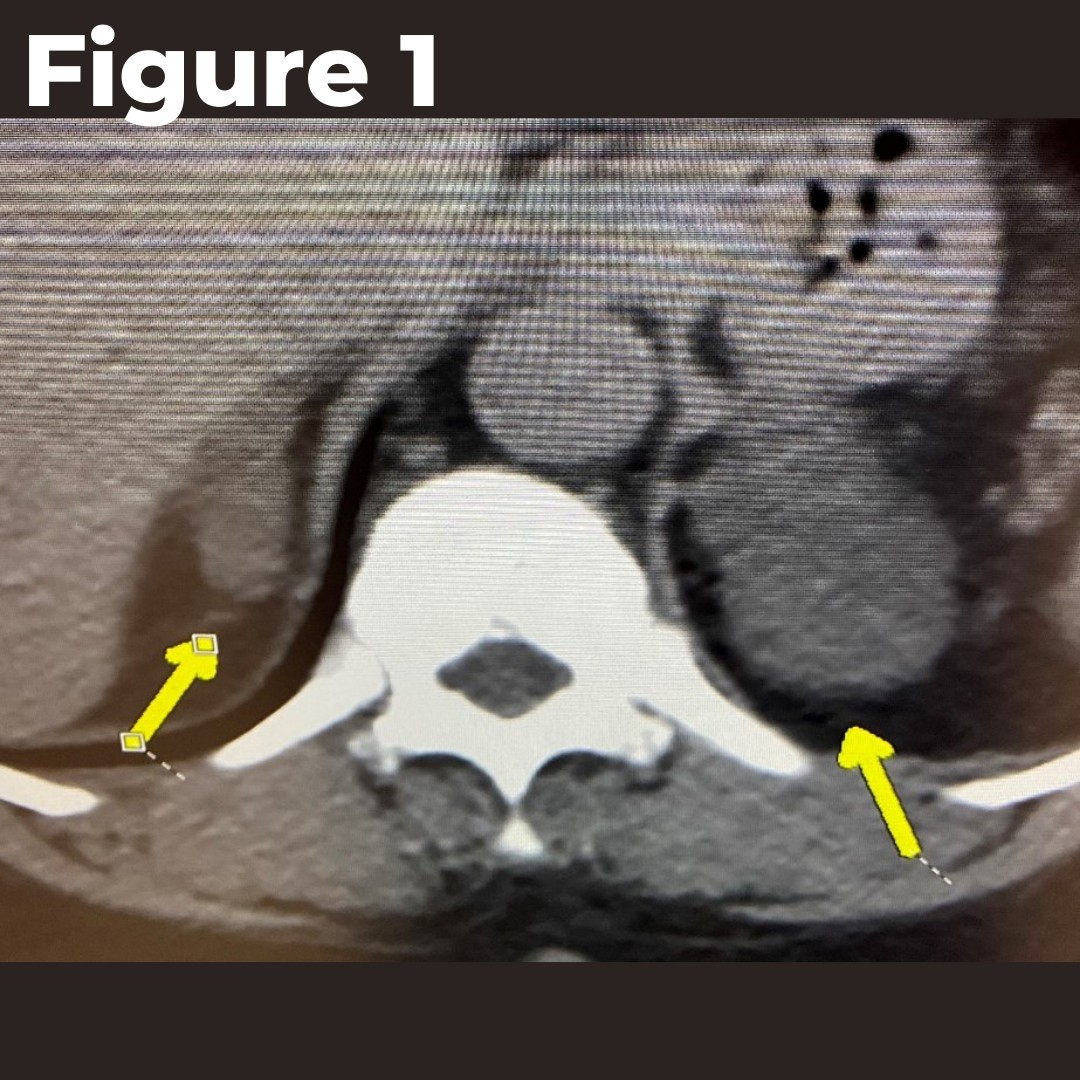
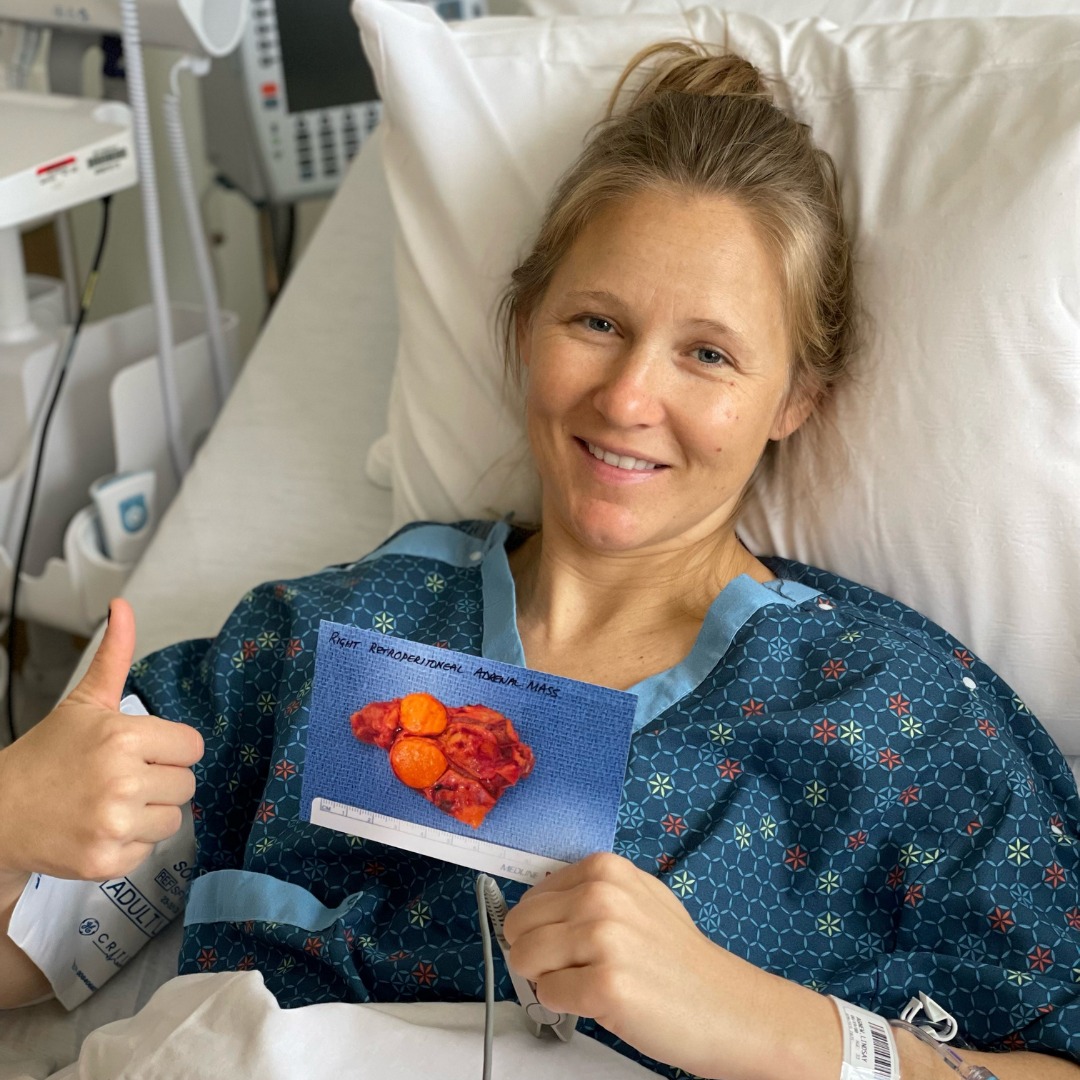
She had undergone a CT scan which showed a right adrenal tumor (Figure 1).
The patient underwent a 15-minute Mini Back Scope Adrenalectomy (MBSA) on the right side. Very soon, the patient felt much better!
Interesting case of the week: AVS is helpful in Conn's syndrome patient
Today's patient is a 69-year-old man with high blood pressure, low blood potassium, leg or arm cramps, muscle weakness, difficulty concentrating, Irritability, anxiety, and depression.
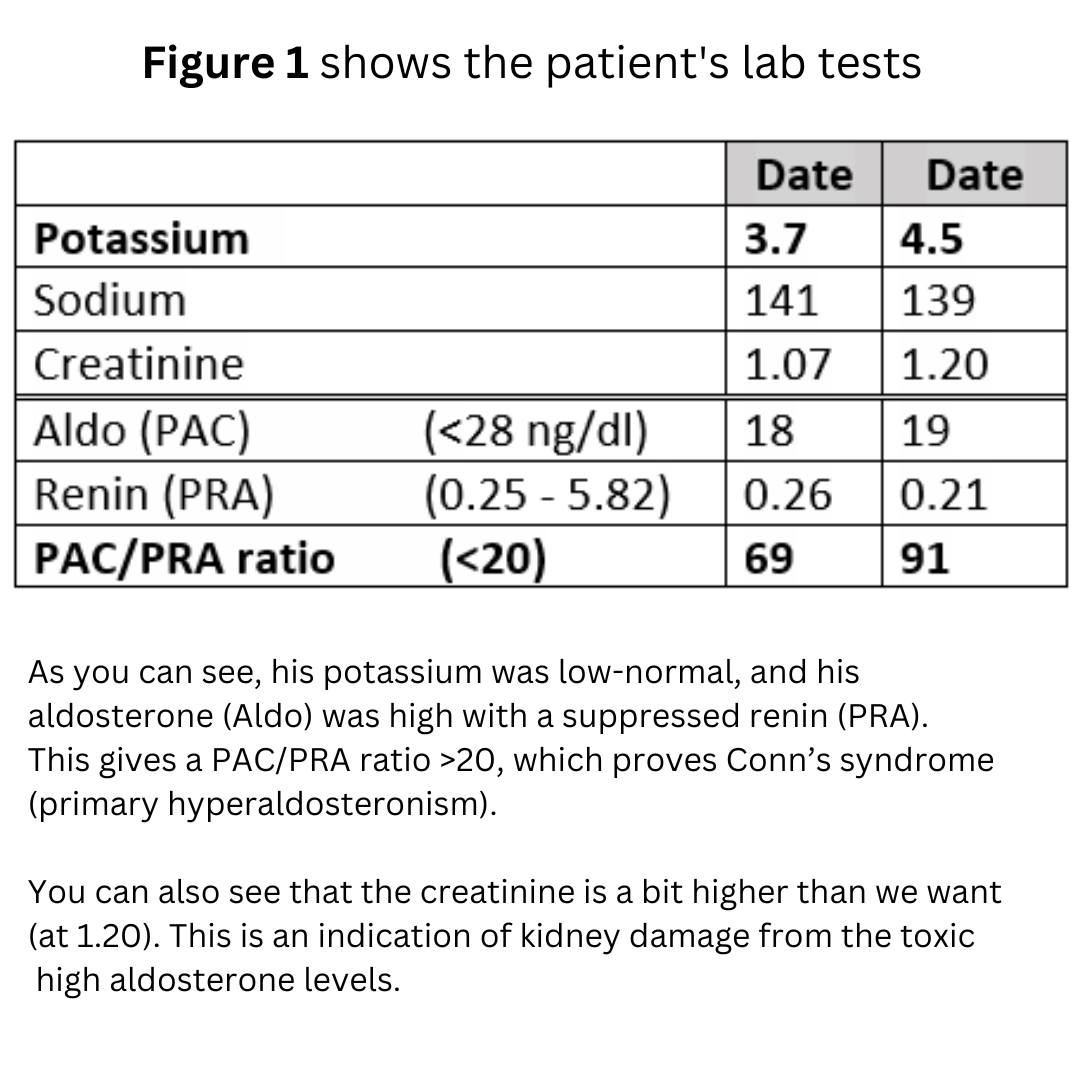
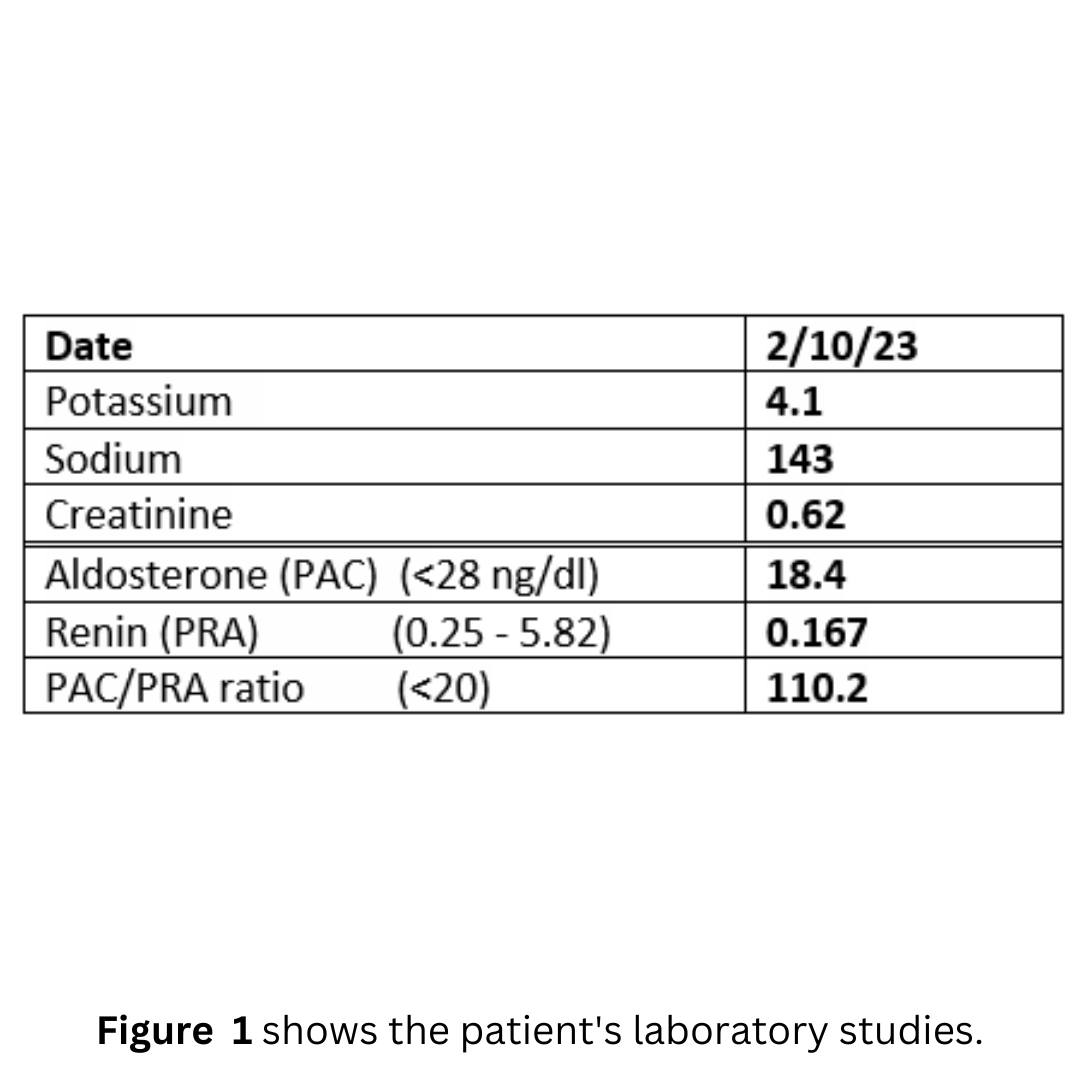
Fortunately, he met a very smart doctor, who worked him up appropriately. You can see his lab results in Figure 1.
He then had a CT scan of his adrenal glands which was read as normal (it wasn’t completely normal as you will see), but he then underwent adrenal vein sampling with Dr. Patel here with us at South Tampa. Dr. Patel now performs more adrenal vein sampling procedures than any interventional radiologist in the country.
You already know that adrenal vein sampling (a procedure to measure aldosterone production from each adrenal gland) has many drawbacks, and in many cases delays curative adrenal surgery.
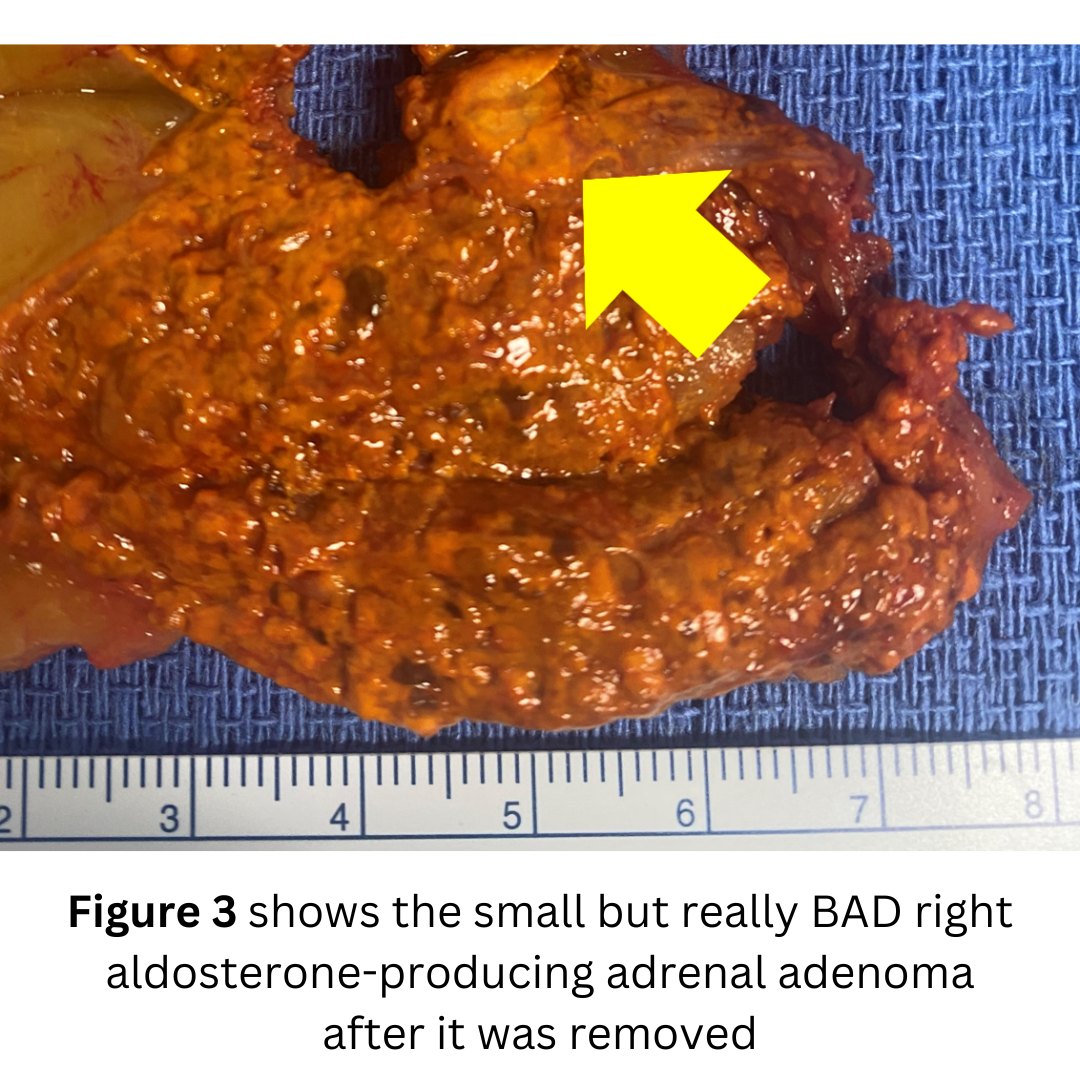
However, this case is an exception in which adrenal vein sampling was very helpful. It demonstrated that the right adrenal gland tumor was the culprit. The right aldosterone-producing tumor was secreting >10 times as much aldosterone (what we called the lateralization index)
As you can see, he actually had a tumor on his right adrenal gland CT scan which showed a tumor on each adrenal gland.
The patient had a left mini back scope adrenalectomy (MBSA) that did take 19 minutes.
His blood pressure normalized very quickly and will continue to improve over the next several weeks.
Interesting case of the week: Subclinical Cushing's syndrome due to right adrenal tumor
Many patients have subclinical Cushing’s syndrome due to an adrenal tumor, and only a fraction are properly diagnosed and treated.
When you have subclinical Cushing’s syndrome it’s due to a tumor of the adrenal gland (or tumors of both adrenal glands, bilateral disease) that produces too much cortisol. Too much and toxic levels of cortisol can cause a lot of symptoms.
Today's patient is a 39-year-old female with the following symptoms: heartburn, heart palpitations, muscle weakness, difficulty concentrating, difficulty with memory, irritability or crankiness, easy bruising, thin skin, poor wound healing, stretch marks on the lower abdomen and upper thighs, anxiety, excessive hair loss, tremor, and panic attack symptoms.
The patient had a mini back scope adrenalectomy that took just16 minutes. She did very well, and we anticipate her to do great and reverse a lot of the detrimental effects of the cortisol overproduction.
Interesting case of the week: Adrenal metastasis in lung cancer survivor
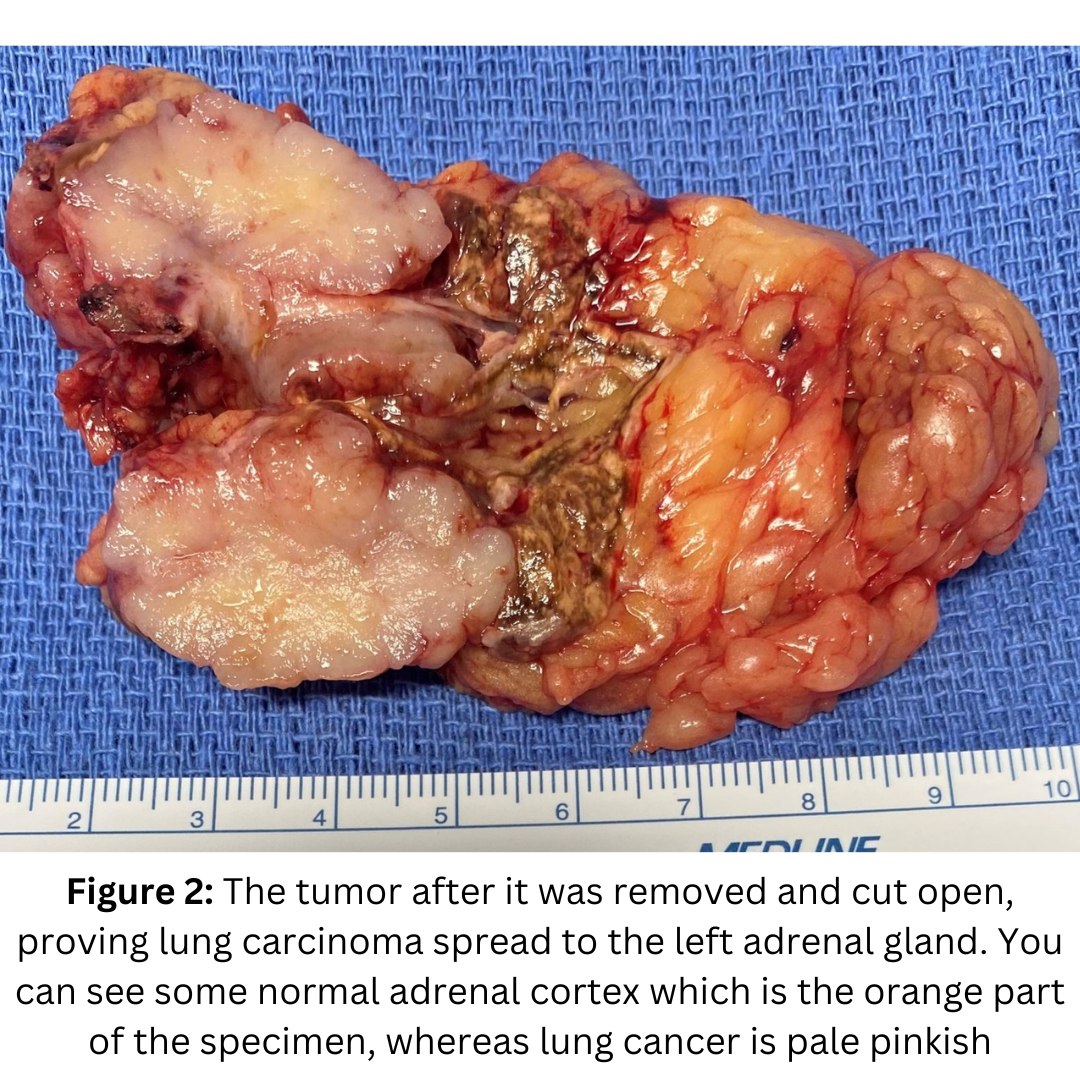
Today's patient is a 75-year-old Florida man. He was recently diagnosed with lung cancer and underwent lung resection. He was doing well overall, but he underwent a PET scan, a left adrenal tumor, consistent with an adrenal metastasis from lung cancer. This caused him to have stage 4 lung cancer. The good news is that there was no other evidence of cancer. His oncologist suggested chemotherapy, but our patient wanted to get rid of the cancer.
He contacted Dr. Carling at the Carling Adrenal Center to see if it would be feasible to remove the left adrenal metastasis (originating from the lung cancer) via a Mini Back Scope Adrenalectomy.
Dr. Carling reviewed his case and given that this was the only site of cancer, surgery is definitely the best option.
He had an uncomplicated 22 minute left Mini Back Scope Adrenalectomy. Sometimes adrenal metastasis can be very inflamed and stuck to other tissues making the operation technically challenging. Fortunately, this tumor came out without too much of a fight.
He will continue to be closely followed by his local oncologist. His biggest wish is to see his grandkids graduate high school. He was very appreciative to have another shot at life!
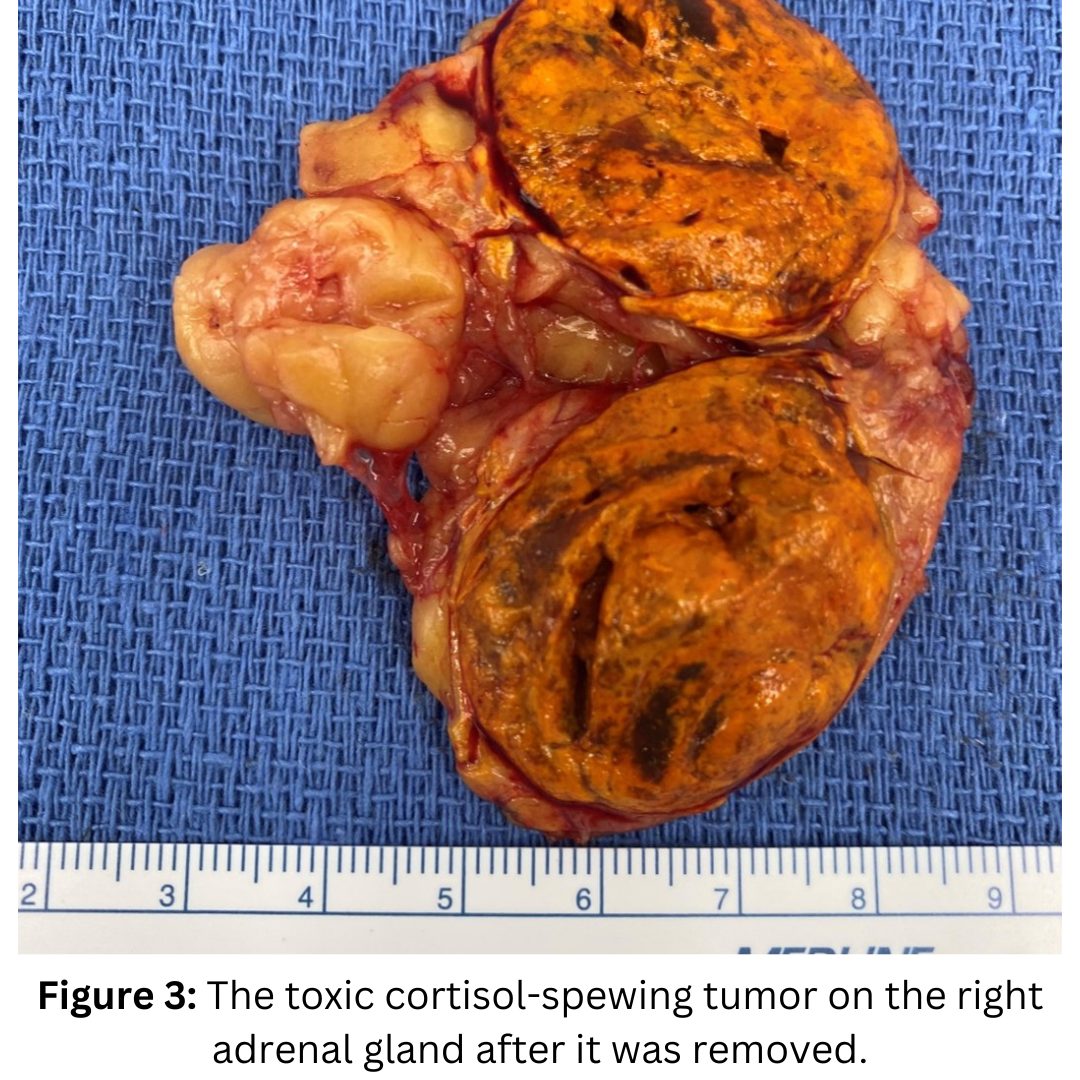
Interesting case of the week: Severe Cushing's syndrome in Tennessee mom
Subclinical Cushing’s syndrome is more common than overt or severe Cushing’s syndrome. The difference is that the latter has a more rapid onset, and the cortisol levels are much higher leading to rapidly progressing symptoms. Cushing’s syndrome on steroids! Pardon the pun. The steroid hormone (cortisol) is the problem.
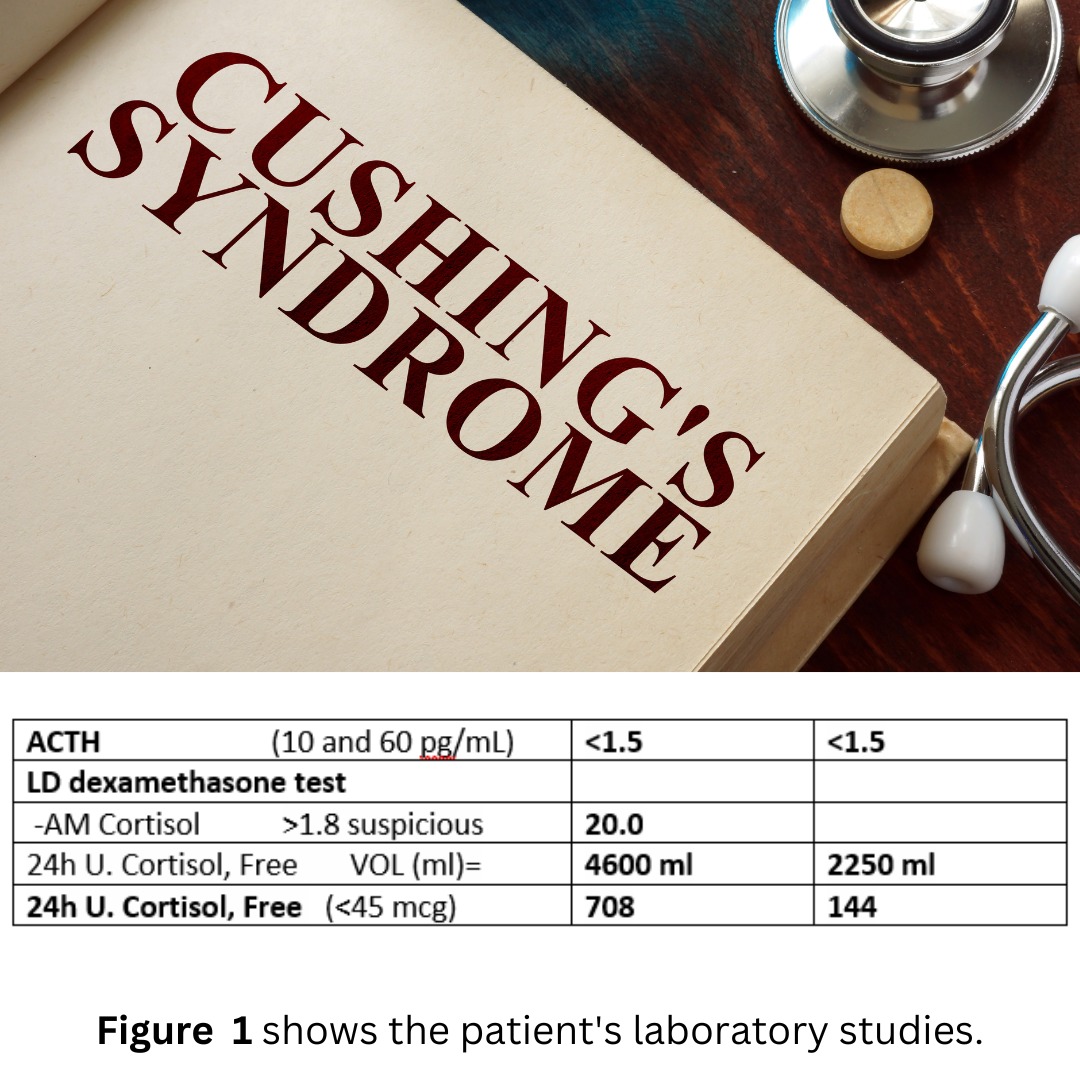
Today's patient is a 41-year-old mom from Tennessee who suffered from rapidly worsening symptoms of high blood pressure, leg and arm cramps, muscle weakness, decreased sex drive, difficulty with concentration, moon face, irritability, supraclavicular and dorsocervical fat pads (buffalo hump), excessive hair loss, weight gain with central obesity.
Fortunately, her endocrinologist took her seriously, and measured her cortisol levels. The cortisol in the urine was so high that the doctor thought it was a lab error. They checked it again and it was still high.
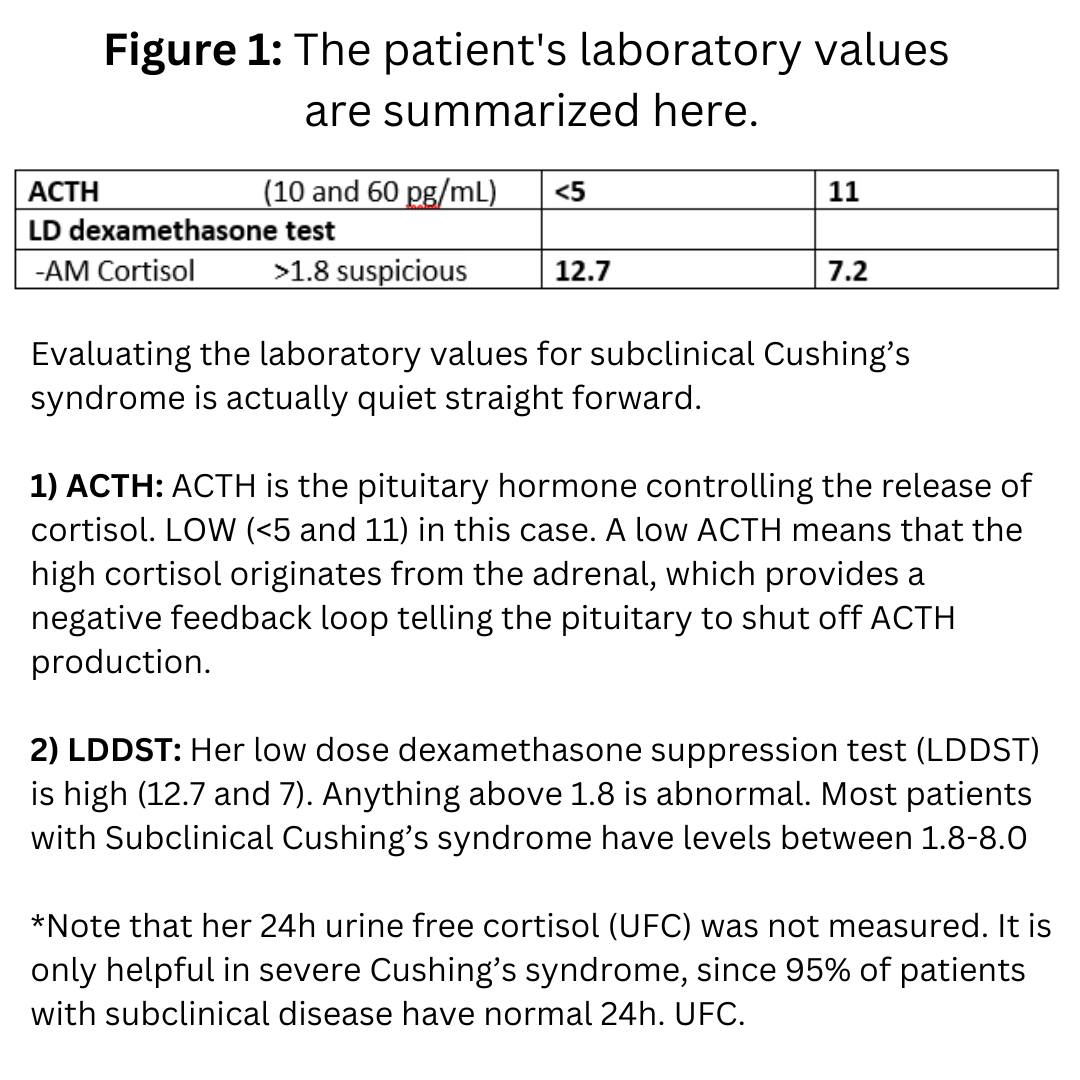
Her laboratory values are shown in Figure 1.
Evaluating the laboratory values for severe and subclinical Cushing’s syndrome is actually quite straightforward. However, you would not believe how many doctors manage to get themselves and the patients confused.
1) ACTH. ACTH is the pituitary hormone controlling the release of cortisol. LOW (<1.5) in this case. A low ACTH means that the high cortisol originates from the adrenal, which provides a negative feedback loop telling the pituitary to shut off ACTH production. A low ACTH means an adrenal cause of excess cortisol. PERIOD.
2) Her low dose dexamethasone suppression test (LDDST) is high (20). Anything above 1.8 is abnormal. 20 is super high, and consistent with severe Cushing’s syndrome. Most patients with Subclinical Cushing’s syndrome have levels between 1.8-8.0
3) Her 24h. urine free cortisol (UFC) is super high at 708, then repeated at 144. Again, consistent with severe Cushing’s syndrome. Normal is <45. 95 % of patients with Subclinical Cushing’s syndrome have NORMAL 24h. urine free cortisol (UFC). Super important to know! Only severe patients have high urine cortisol levels. If I had a penny for every time a patient had been told by their doctor that they can’t have Cushing’s syndrome because their urine cortisol is normal… It is only high in the worst 5% of cases.
She had a right mini back scope adrenalectomy (MBSA) that took about 17 minutes and did very well. Her hair will soon grow back, the blood pressure normalizes, the weight will come off, and her energy will increase. She is a brave mama, and she needs all the energy she can get!
Interesting case of the week: Conn' syndrome in flight attendant
We see a fair number of patients who are airline pilots and flight attendants. The reason for this is that they have strict health controls and screenings, including blood pressure measurements to make sure they are able to fly safely.
Since high blood pressure is one of the most common and first symptoms of an adrenal tumor, it may be detected early in those who have their blood pressure checked regularly.
Today's patient is a 60-year-old flight attendant. She was otherwise healthy and slender. She was a textbook case of Conn’s syndrome (primary hyperaldosteronism), but like many patients, it took a long time to arrive at the correct diagnosis. In addition to high blood pressure, she had muscle cramping, decreased sex drive, difficulty concentrating, difficulty with memory and irritability.
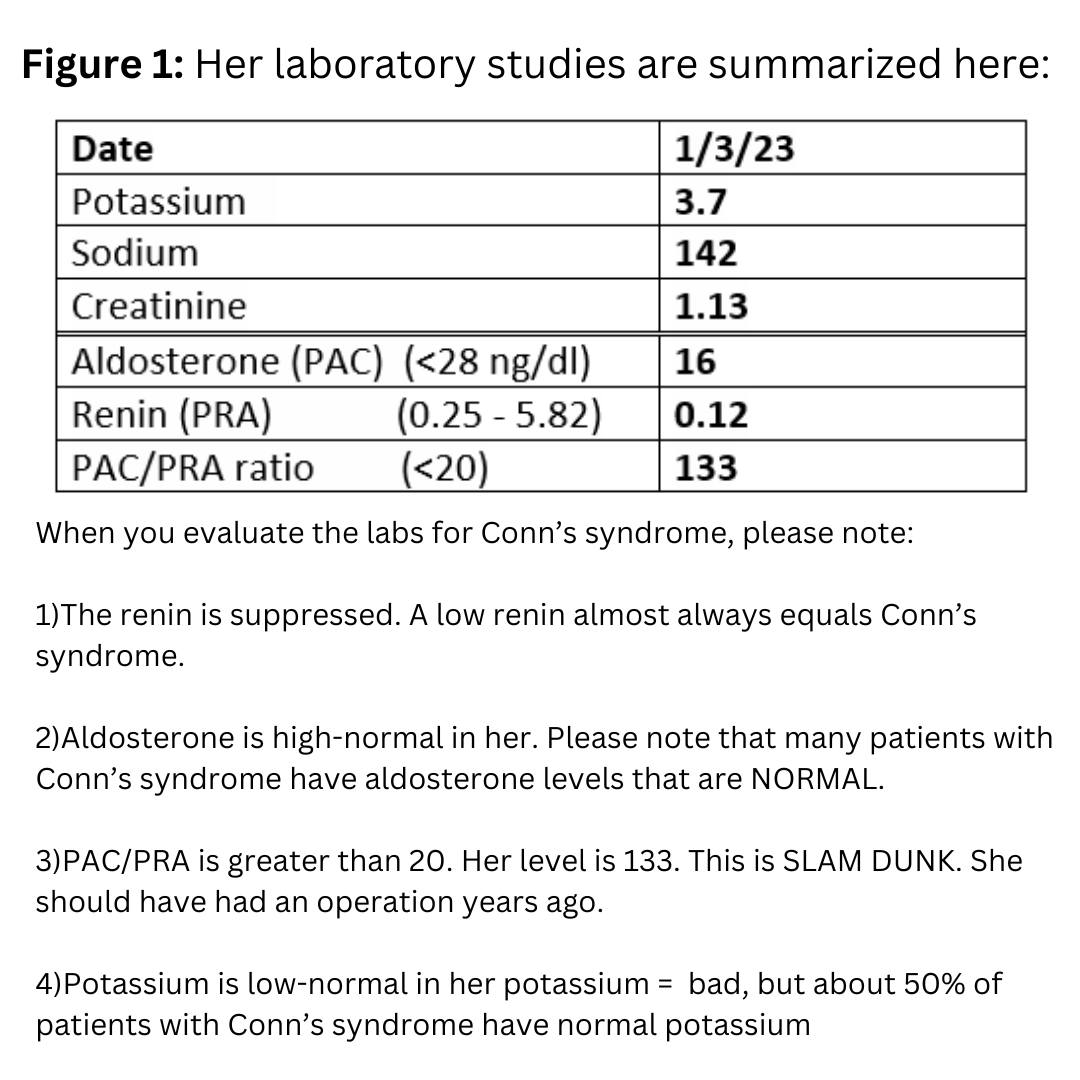
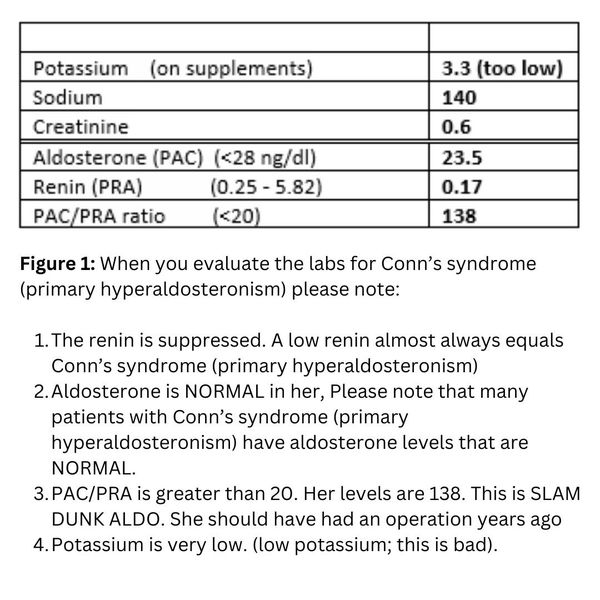
Her laboratory studies are summarized here in Figure 1.
When you evaluate the labs for Conn’s syndrome (primary hyperaldosteronism) please note
1) The renin is suppressed. A low renin almost always equals Conn’s syndrome (primary hyperaldosteronism)
2) Aldosterone is high-normal in her. Please note that many patients with Conn’s syndrome (primary hyperaldosteronism) have aldosterone levels that are NORMAL.
3) PAC/PRA is greater than 20. Her level is 110. This is SLAM DUNK ALDO. She should have had an operation years ago…
4) Potassium is normal in her. Low potassium = bad, but about 50% of patients with Conn’s syndrome have normal potassium
The patient had a swift 18-minute left mini back scope adrenalectomy (MBSA). The patient did very well. She is already back in the air, and cured from her Conn’s syndrome!
Interesting case of the week: Silent Pheo in Anesthesia Doctor
Anesthesiologists are the doctors who take care of the patient while they sleep during an operation. No one knows better that you have to find the best surgeon in the world for your operation, than an anesthesiologist. Anesthesia doctors have seen it all. If they get sick, they want the very best and most experienced surgeon.
Today's patient is a 46-year-old anesthesia doctor from Texas. He was completely asymptomatic, but did have a history of heartburn and hypertension (even though he was slender, relatively young and active) requiring 2 blood pressure medications.
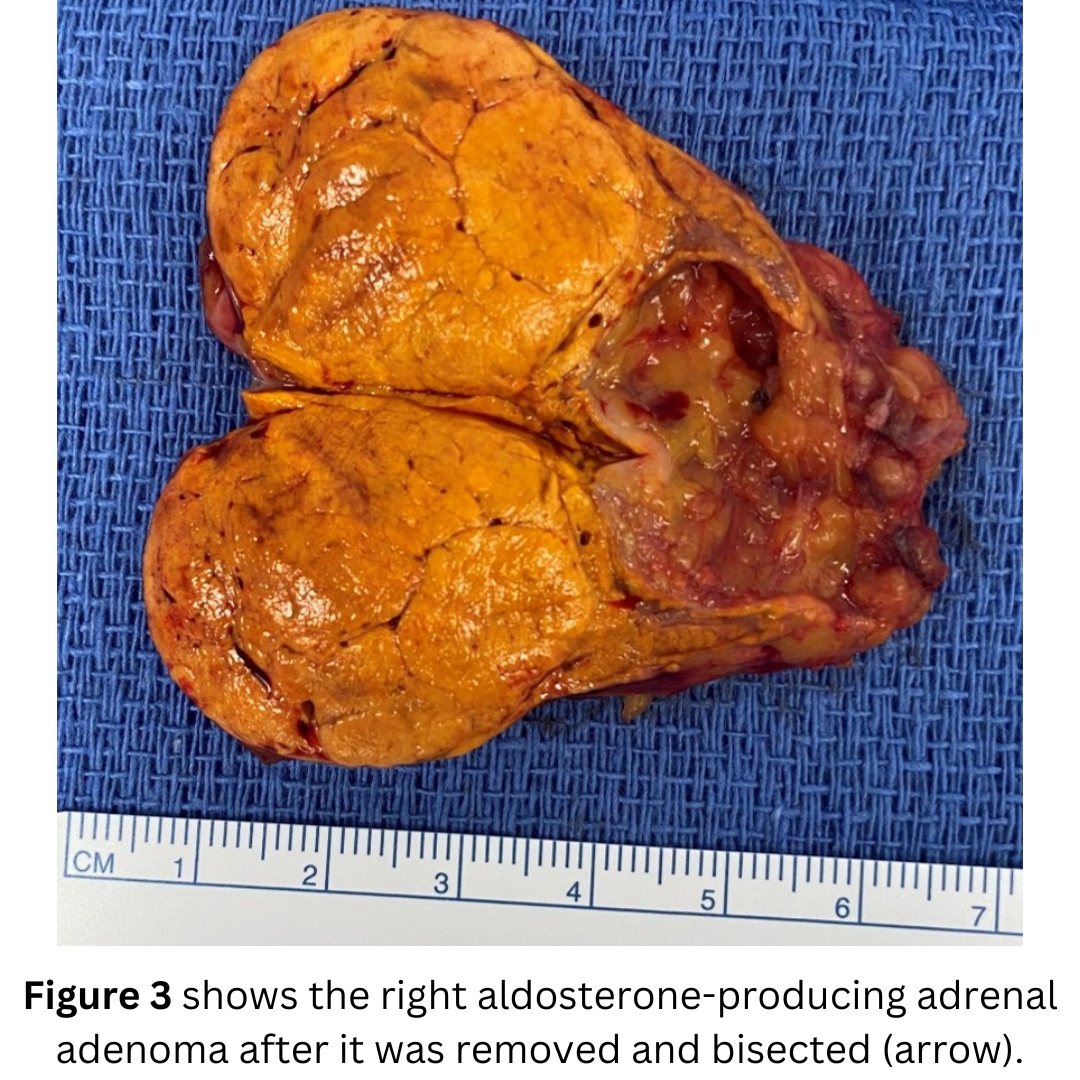
He had undergone a CT scan for unrelated reasons, and this showed a 4.9 cm right adrenal mass. It appeared indeterminate. It had an “atypical imaging phenotype”. This means it did not look like a typical benign adrenal adenoma.
The patient’s plasma and 24-hour urine catecholamines were all normal. All other lab test were normal as well. Fortunately, he reached out to us at the Carling Adrenal Center and we took it very seriously.
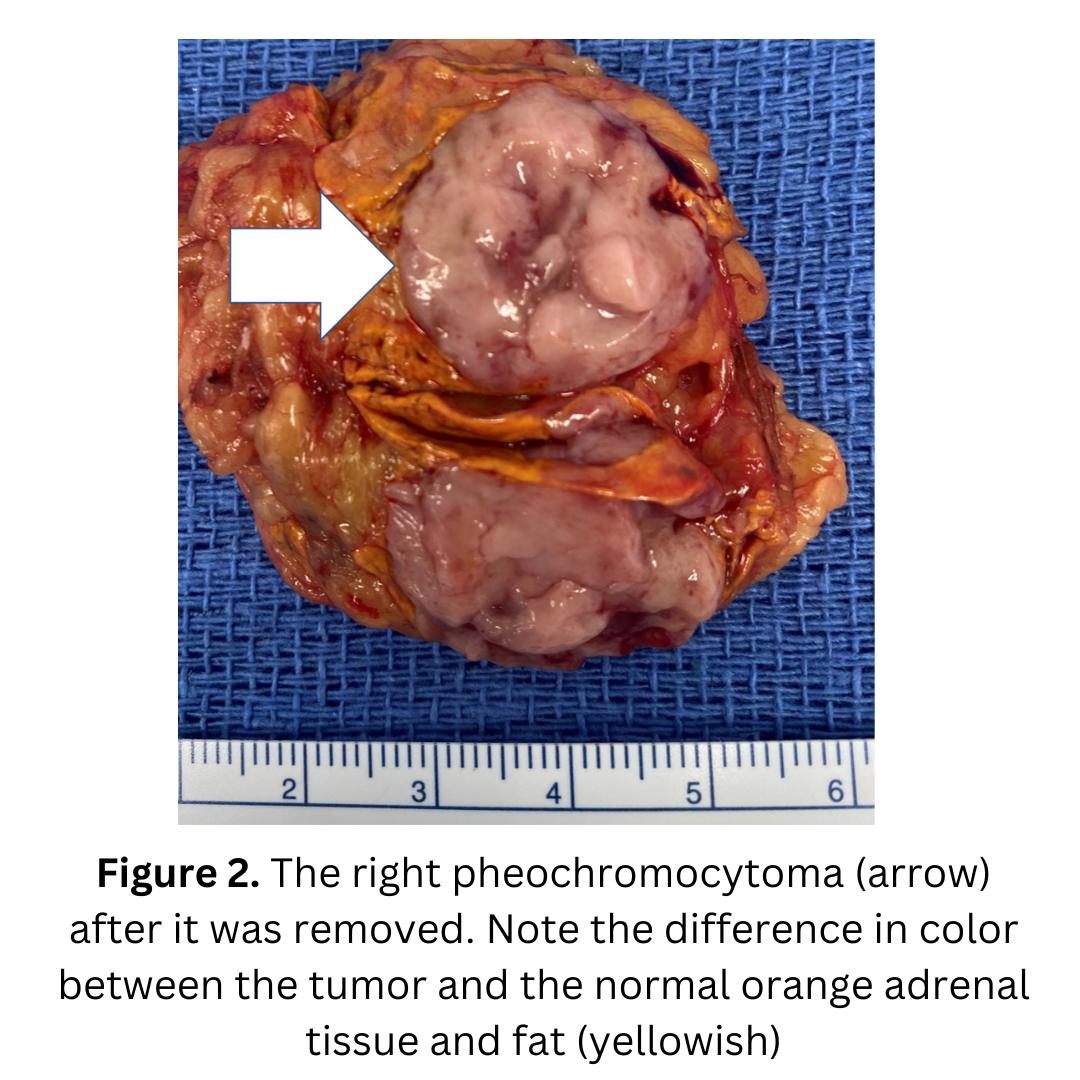
The patient had a very swift 21-minute left mini back scope adrenalectomy (MBSA). A few days later we got the best possible call from the pathologist. Indeed, this anesthesia doctor from Texas had a “silent” pheochromocytoma. This means that the pheochromocytoma was normo-hormonal, meaning it did not produce so much hormone that it was elevated in the blood or urine tests. This is rare, but Dr. Carling has seen several given his high volume.
Pheochromocytomas can be tricky to diagnose, and it is even trickier if the hormone levels are normal, or almost normal.
The patient did great, and when Dr. Carling called him a few days after the operation, he was already in the operating room himself working. Typical doctors!
Adrenal surgery for all tumors, and especially for pheochromocytoma is definitely worth travelling for!
Interesting case of the week: Primary hyperaldosteronism in patent from New Zealand
There are a lot of doctors and other healthcare providers that do not know enough about Conn’s syndrome and primary hyperaldosteronism. This is not only true in America, but all over the world. Many doctors think it is a rare disease and that adrenal tumors do not need to be taken seriously.
This patient came to us all the way from New Zealand. She is the first patient with an adrenal tumor from New Zealand to be operated on at the brand-new Hospital for Endocrine surgery. (We just celebrated our 1 year anniversary!)
When you have Conn’s syndrome, it’s due to a tumor of the adrenal gland that is producing too much aldosterone. Too much and toxic levels of aldosterone can cause a lot of symptoms.
The patient had a “slum dunk” diagnosis of primary hyperaldosteronism and Conn’s syndrome. The lab tests showed that:
1) The renin is suppressed. A low renin almost always equals Conn’s syndrome (primary hyperaldosteronism)
2) Aldosterone was high (Please note that many patients with Conn’s syndrome have aldosterone levels are in the normal range.
3) Aldosterone divided by renin (PAC/PRA) was greater than 20.
4) Potassium is very low. (low potassium; this is bad).
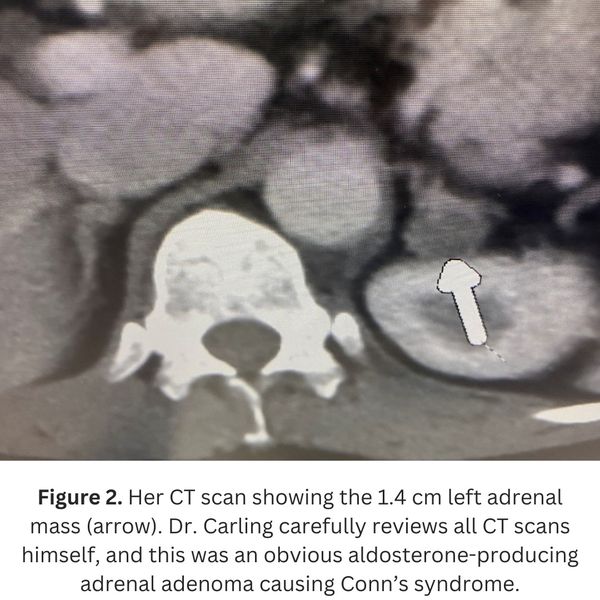
The New Zealand doctors had obtained a CT scan which showed a classic left 1.4 cm adrenal tumor. So…they referred her straight for surgery, correct? No, they did not. Instead, they sent her for adrenal vein sampling (AVS). The AVS failed, not once, but 2 times!
So the New Zealand doctors through their hands up in the air, and said, “Well I guess we just put you on one blood pressure pill after another for the next few decades until you have a stroke, kidney failure or a heart attack”. Okay -- we are exaggerating, but that would be the consequence. This is when our patient contacted the Carling Adrenal Center
The patient had a mini back scope adrenalectomy that took 17 minutes. Can you imagine traveling for two days to have a 17-minute operation? Well trust us, it’s a lot better than being put you on one blood pressure pill after another for the next few decades until you have a stroke, kidney failure or a heart attack.
The patient is completely cured of her Conn’s syndrome and is off all blood pressure medications and the large potassium pills she had to take for her low potassium.
Interesting case of the week: Recurrent Pheo in MEN2
Pheochromocytomas may occur in the familial (genetic) setting. As you know, adrenal tumors may arise in genetic endocrine tumor susceptibility syndromes, such as multiple endocrine neoplasia, von Hippel Lindau, and neurofibromatosis type 1 disease.
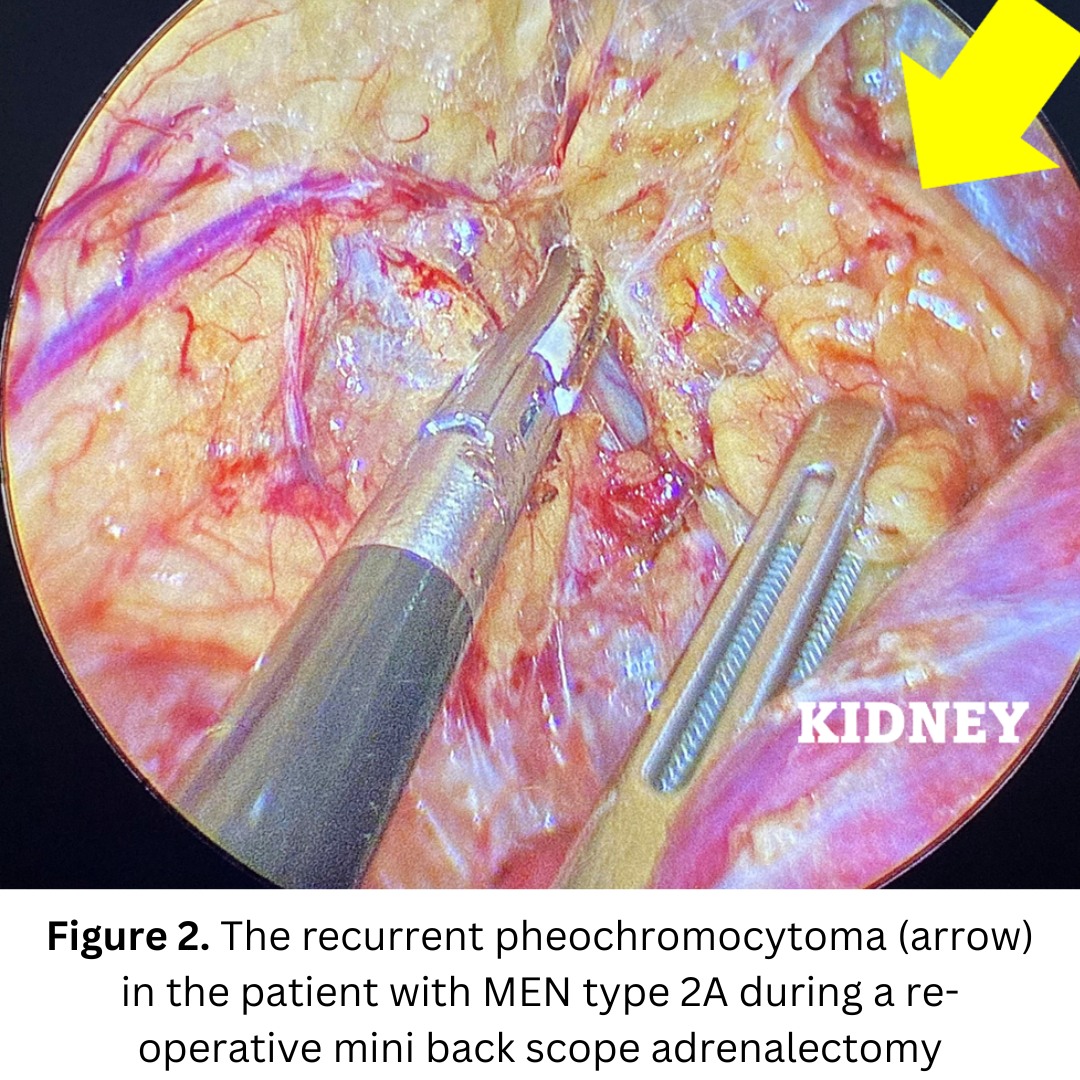
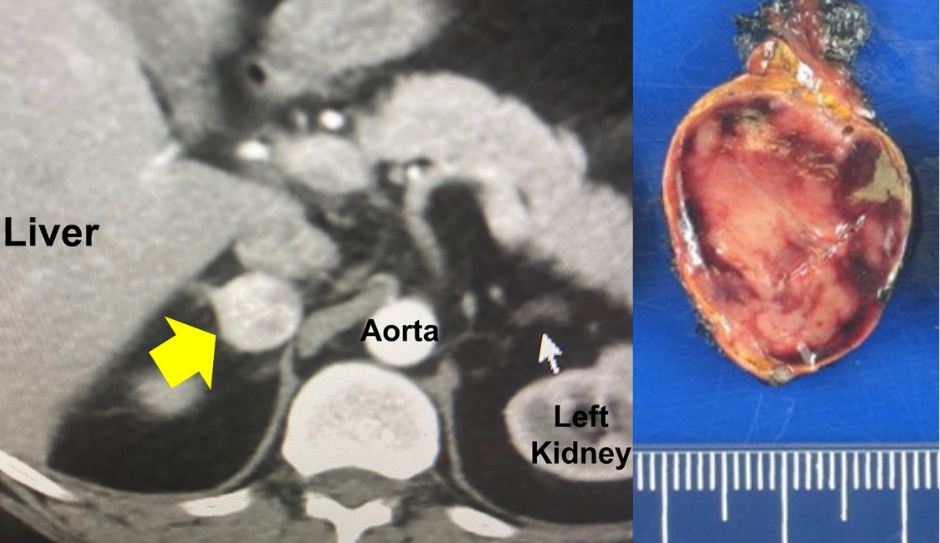
Today's patient is a 37-year-old woman who has had a long-standing diagnosis of multiple endocrine neoplasia type 2A. This disease is a known tumor susceptibility syndrome, making her prone to develop pheochromocytomas. It is due to a genetic mutation in the gene RET. Classically, patients can also develop medullary thyroid cancer and parathyroid tumors.
These patients tend to develop pheochromocytomas, often on both adrenal glands. That’s exactly what this patient had. In fact, the patient had already undergone a complete total bilateral adrenalectomy several years ago. This meant that she had no adrenal tissue and was dependent on taking daily steroids.
However, now her pheochromocytoma symptoms had come back. How is this possible? She has no adrenal glands, right? Well…her previous surgeon lacked experience and had actually left adrenal tissue and adrenal tumor tissue behind.
The pheochromocytoma grew back.
It is never ideal to have to perform a re-operation because the second time around there is more scar tissue and the tumor may be stuck to important surrounding structures.
The patient underwent a 21-minute left mini back scope adrenalectomy (MBSA). She did very well and is now cured.
The Hospital for Endocrine Surgery is the only hospital in the world dedicated to the surgical treatment of adrenal, thyroid, and parathyroid disease.
Interesting case of the week: Adrenal Incidentaloma in Radiology Doctor
What is an Adrenal Incidentaloma? The definition of an adrenal incidentaloma (sometimes termed adrenal mass, or nodule) is an adrenal lesion that is discovered when a radiological (X-ray) study (often CT or MRI) is performed for indications other than for adrenal disease (e.g., belly pain, car accident, etc.). That means it was discovered incidentally, or by accident.
All adrenal incidentalomas need to be taking seriously, since they can be cancerous or overproduce hormones (as in Cushing’s syndrome, Conn’s syndrome and pheochromocytoma).
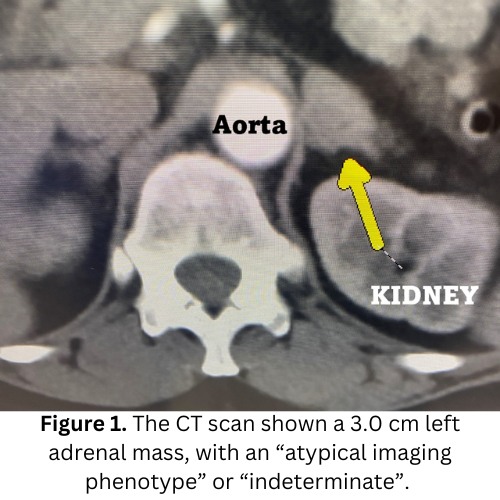
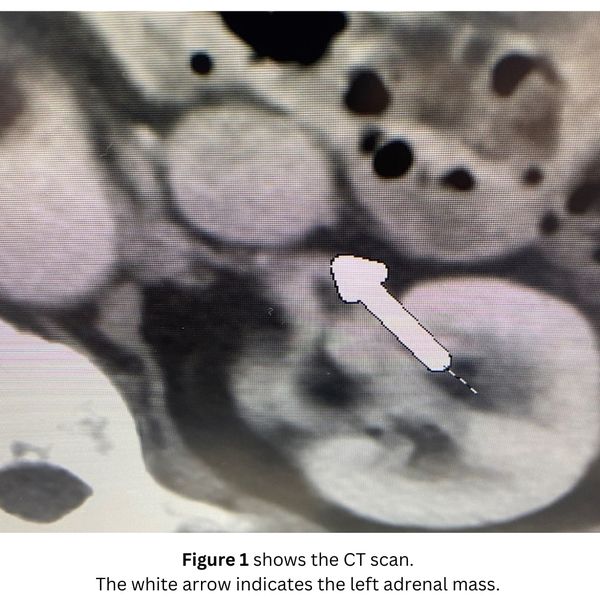
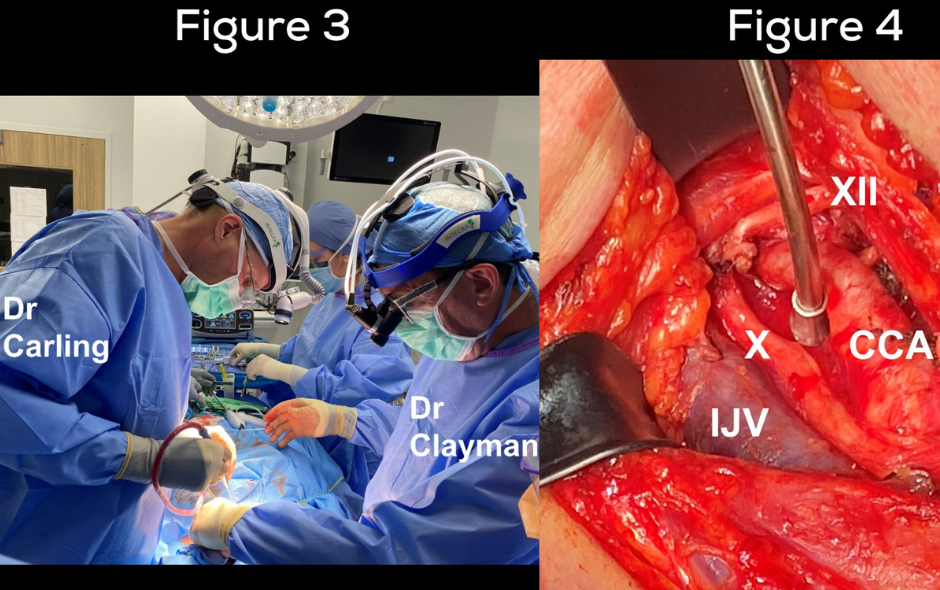
Today's patient is a 59-year-old radiologist. In fact, she is a Professor of Radiology at one of the most prestigious Ivy league university hospitals in the world. She had looked at thousands of adrenal masses during her career, but now it hit home. Her own scan showing an adrenal tumor is shown in Figure 1.
All of her hormones were checked and were normal. There was no concern for Cushing’s syndrome, Conn’s syndrome or pheochromocytoma.
She also showed her scan to all her radiology colleagues, and they all agreed that her tumor was atypical or indeterminate.
So, what did this radiologist want to do with her atypical adrenal tumor? Have another scan in 6-12 months to see if it would grow? No way -- she wanted her tumor out, ideally yesterday!
She contacted us here at the Carling Adrenal Center and we rapidly got her ready for surgery. The patient had a very swift 18-minute mini back scope adrenalectomy (MBSA) and is doing great! A few days later, we got the best phone call from the pathologist. The tumor turned out to be an adrenocortical adenoma, meaning a non-cancerous adrenal tumor
Interesting case of the week: Adrenal metastasis in Maryland Professor
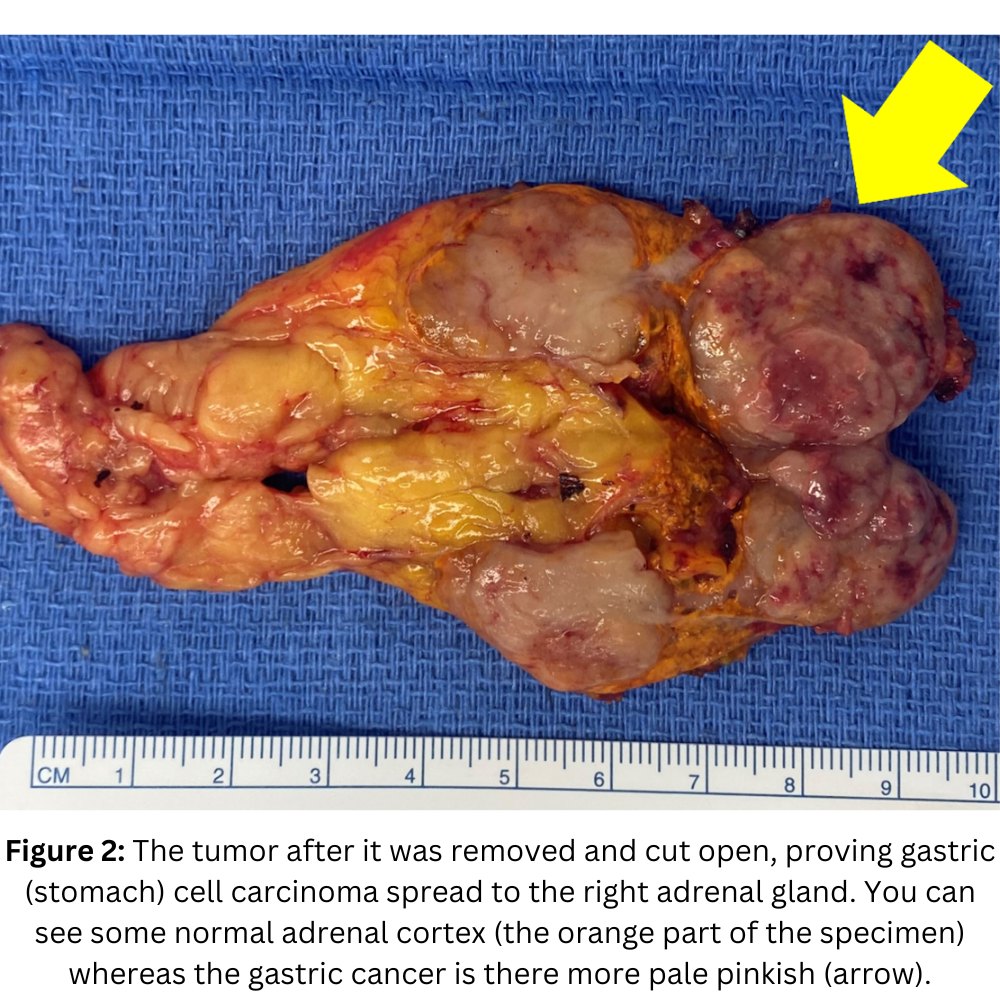
Today's patient is a 75-year-old professor from Maryland. He has Stage 4 stomach (gastric) cancer. About 2 years ago, he underwent e a partial gastrectomy as well as HIPEC treatment. HIPEC treatment is an advanced cancer treatment where hot chemotherapy is infused into the abdominal cavity. This can be effective in aggressive cancers, but it does cause significant scarring in the belly, making future surgery much more challenging and sometimes impossible.
Initially after the operation, he was doing well. He was under the care of a medical oncologist (cancer doctor) and was followed with multiple scans.
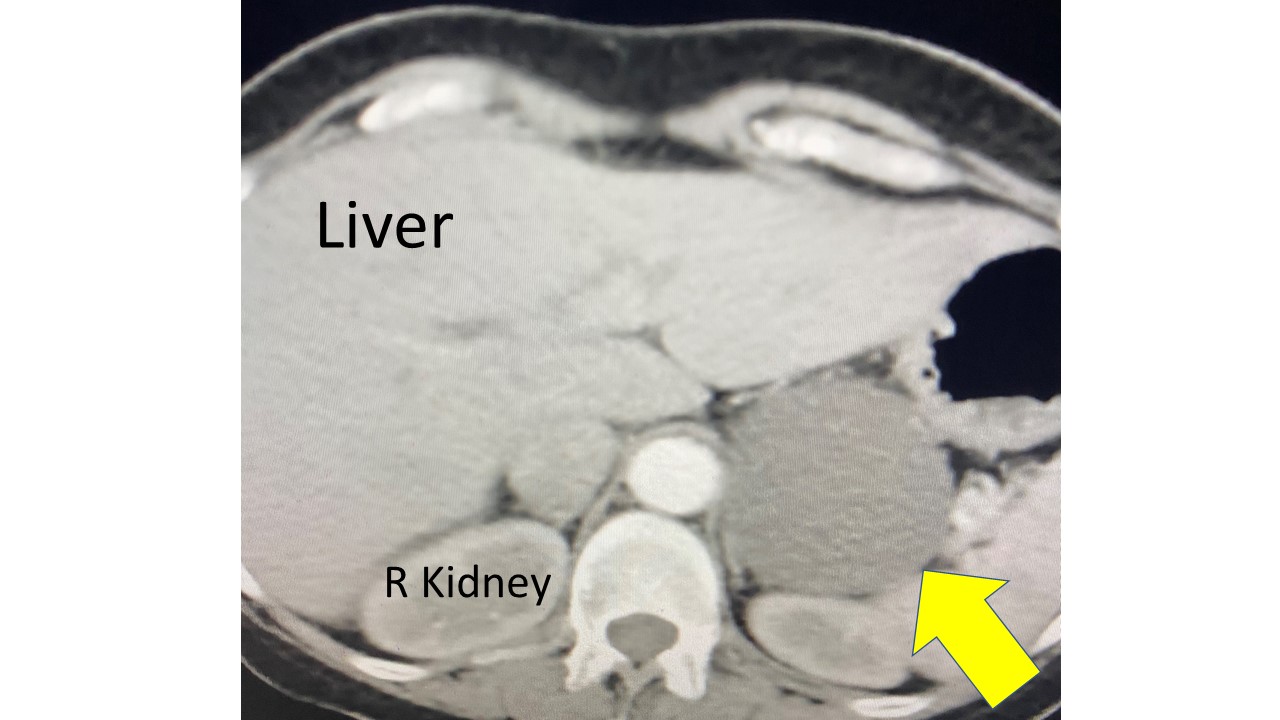
On the most recent scan (MRI), unfortunately, a new mass in the left adrenal gland was noticed. Initially it was not acted on as it was as small as 2.1 cm, but it did continue to grow. Thus, he underwent a PET scan, which again showed this tumor, consistent with an adrenal metastasis from the gastric cancer. Importantly, there was no other evidence of cancer.
He contacted Dr. Carling at the Carling Adrenal Center, to see if it would be feasible to remove the left adrenal metastasis via a Mini Back Scope Adrenalectomy. Remember, this surgery is always better then going through the belly. In this patient especially so, since his entire abdomen is scarred in from the HIPEC treatment.
He was otherwise feeling well and in a good shape. He had a Mini Back Scope Adrenalectomy (MBSA) and did great. He will continue to be closely followed by his local oncologist in Maryland.
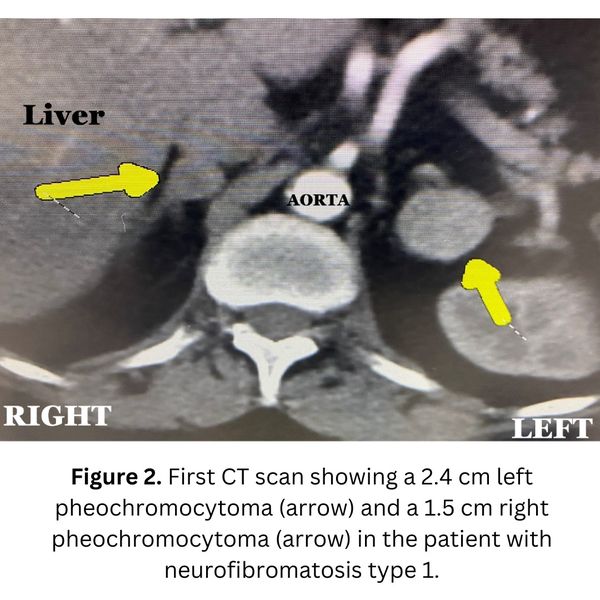
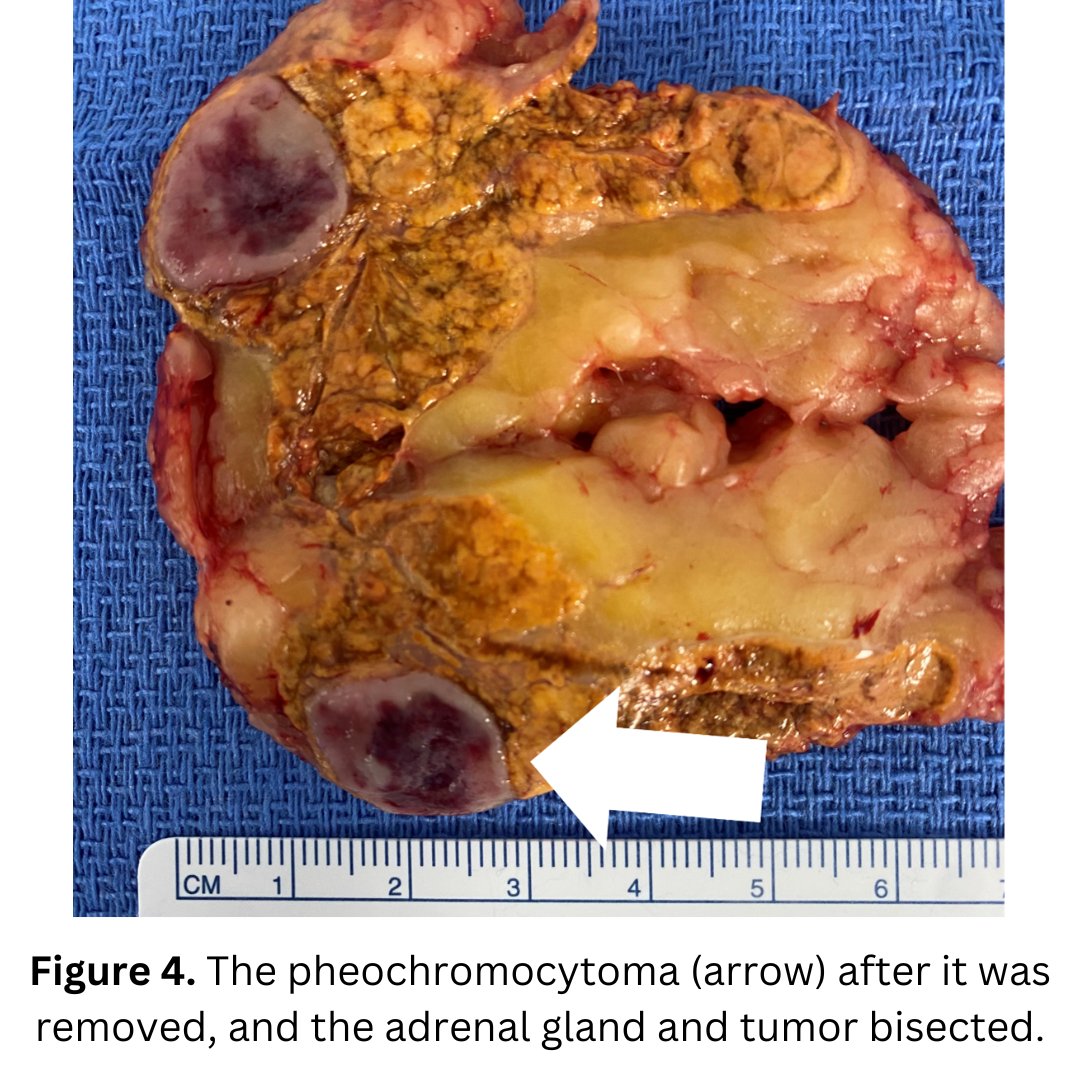
Interesting case of the week: Bilateral pheochromocytomas in neurofibromatosis type 1
Pheochromocytomas may occur in the familial (genetic) setting. As you know, adrenal tumors may arise in genetic endocrine tumor susceptibility syndromes, such as multiple endocrine neoplasia, von Hippel Lindau, and neurofibromatosis type 1 disease.
Today's patient is a 63-year-old woman who has had a long-standing diagnosis neurofibromatosis type 1. This disease is a known tumor susceptibility syndrome making her prone to develop pheochromocytomas. It is due to an inherited mutation in the gene NF1. Classically, patients develop skin lesions, called neurofibromas. These are skin tumors which can occur all over the body.
In addition to these skin tumors (neurofibromas), patients tend to develop pheochromocytomas, often on both adrenal glands. That’s exactly what this patient had. Fortunately, they were not huge, meaning Dr. Carling could remove them and at the same time preserve enough normal adrenal tissue so she does not become adrenal insufficient.
We elected to deal with the left pheochromocytoma first. Fortunately, the tumor was in a low aspect of the adrenal gland, and a partial adrenalectomy was ideal.
The patients did great from the very swift 21-minute left partial mini back scope adrenalectomy (MBSA).
She recovered from surgery, and as you can see from this follow up CT scan her tumor is gone on the left side, but she has a perfect remanent of normal adrenal cortex. The right pheochromocytoma is relatively unchanged from the first CT scan.
Now, it was time to perform a right partial mini back scope adrenalectomy (MBSA).
The patient did great and can put this all behind her!
Interesting case of the week: Cushing's syndrome due to bilateral tumors
This week's patient is a sweet lady from Connecticut with subclinical Cushing’s syndrome due to tumors of both adrenal glands. Dr. Carling spent 17.5 years in Connecticut, and many patients get on an easy flight from Connecticut and all over New England to the Hospital for Endocrine Surgery for their adrenal surgery.
When you have subclinical Cushing’s syndrome, it’s due to a tumor of the adrenal gland (or tumors of both adrenal glands) that is producing too much cortisol. Too much and toxic levels of cortisol can cause a lot of symptoms.
About ¾ have one tumor on one adrenal gland, but ¼ have tumors on both adrenal glands. This confuses a lot of doctors, and they don’t know what to do about this group of patients.
What patients need is to remove all tumor tissue but preserve enough normal adrenal tissue, so they don’t become adrenal insufficient. In other words, they need a PARTIAL, BILATERAL ADRENALECTOMY.
Her CT scan showed a 3.8 cm tumor on the right side and 3.0 cm left adrenal mass. Again, the correct thing is to remove all tumor tissue but preserve enough normal adrenal tissue, so she does not become adrenal insufficient but is also CURED of the subclinical Cushing’s syndrome.
First, she had a partial mini back scope adrenalectomy (MBSA) on the right side in November 2022. By the way, she made friends with 3 other patents that day who were operated on for subclinical Cushing’s syndrome.
This week she came back for a partial mini back scope adrenalectomy (MBSA) on the left adrenal.
She did very well. Her cortisol levels were perfect. Truly a Goldilocks operation. Not too much, not too little. She is cured from the subclinical Cushing’s syndrome, but does not need steroids (prednisone, hydrocortisone)
Interesting case of the week: Utah women with big pheo
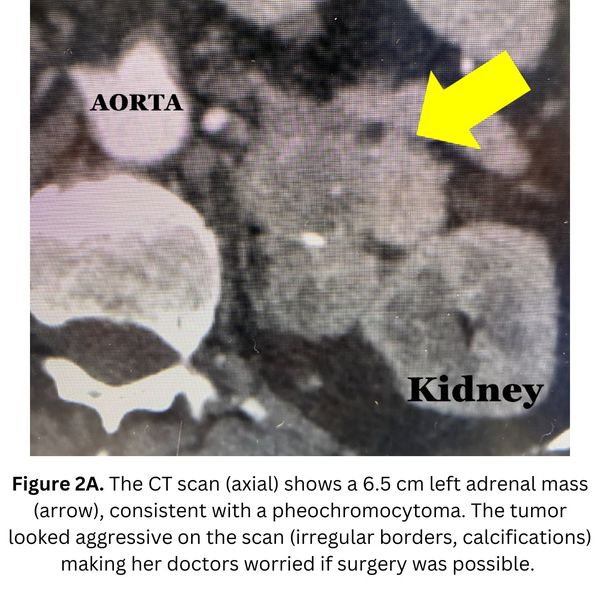
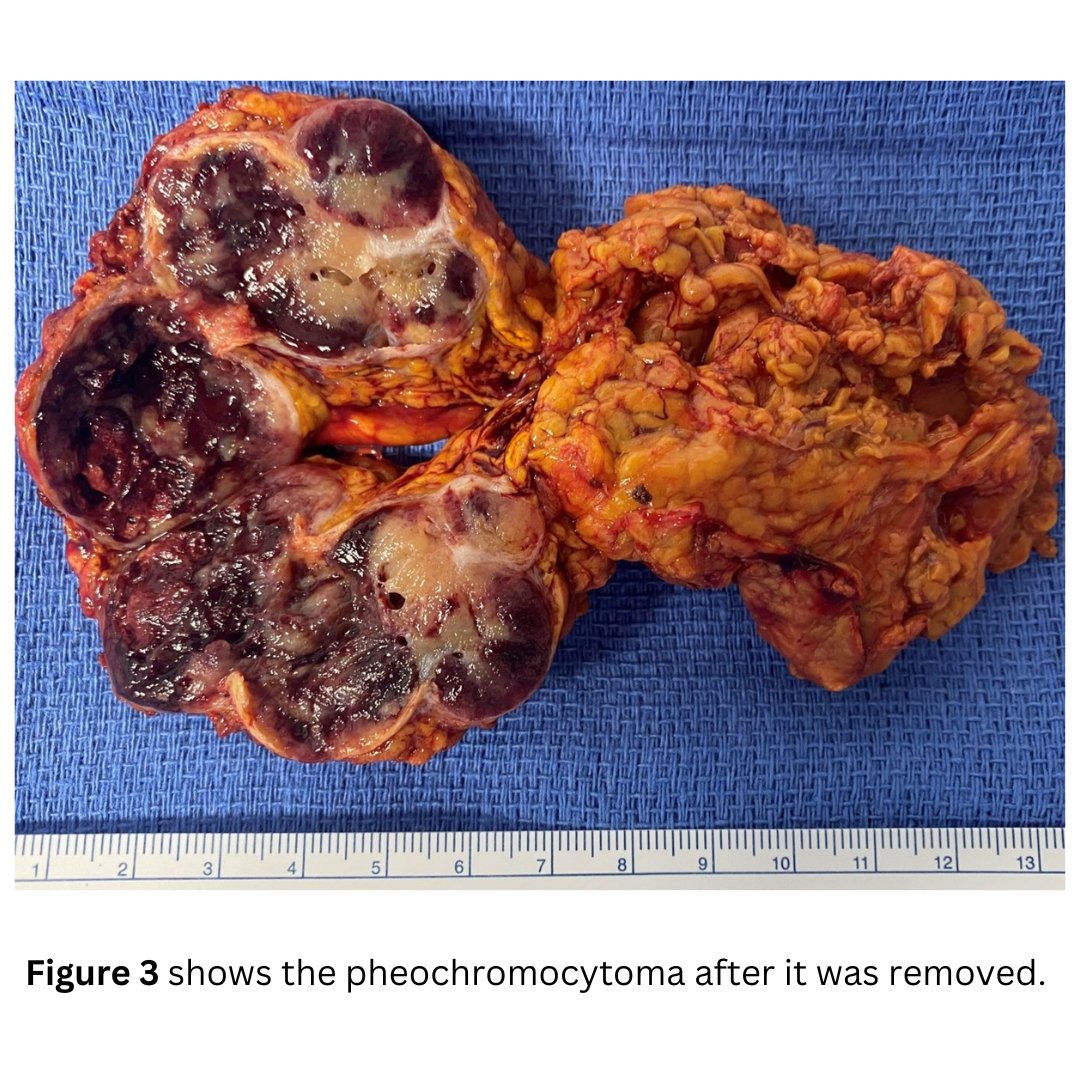
Today's patient is a 58-year-old woman. She underwent a CT scan which revealed a large left adrenal tumor, greater than 6.5 cm, or the size of an orange. In retrospect, she suffered for many years from hypertension, heart palpitations, pre-diabetes, and excessive sweating.
The patient’s 24h Urine metanephrines and normetanephrines were very elevated, proving that she had a pheochromocytoma. The patient started on a medication called prazosin (alpha blocker), and despite this, her blood pressure was very labile.
Despite the obvious diagnosis of pheochromocytoma, her Utah doctors were hesitating. At one point, they recommended everything from chemotherapy to large open operations through the belly, with possible removal of the spleen, pancreas, left kidney, etc. To be fair, there are only slightly more than handful of pheochromocytoma operations performed in Utah per year.
Part of the reason the Utah doctors were nervous about this case was because the tumor looked very nasty and aggressive on the scan. They were worried about cancer, and whether it would even be possible to perform surgery.
Dr. Carling, who operates on multiple pheochromocytoma patients every week, was not as concerned about what the tumor looked like on the scan. His experience has taught him that pheochromocytomas often look aggressive on the scan, but with expert-level skill, they can be removed very safely. Even though the tumor was large, she was a great candidate for the Mini Back Scope Adrenalectomy (MBSA).
The patient did tremendously well. Her blood pressure was cured in the operating room. She was up walking around the day of surgery and will bounce back quickly!
Interesting case of the week: An Alaska Adventurer with Conn's syndrome
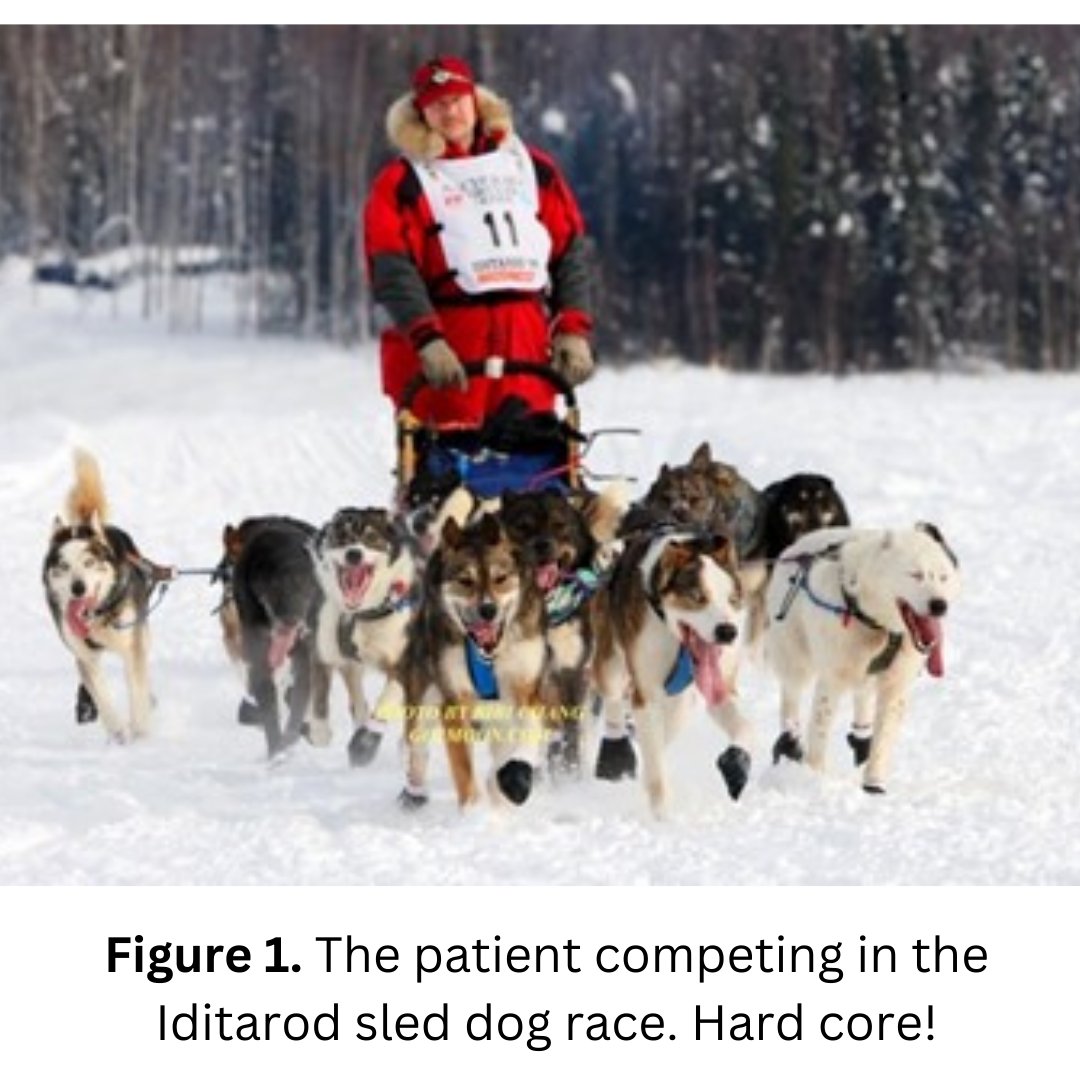
We have the most interesting people come see us in Tampa for their adrenal surgery. It is truly a blessing being able to help patients getting back to health, joyful lives.
This case illustrates how a very small, but very toxic aldosterone producing tumor can cause huge problems in an otherwise strong, healthy man.
Today's patient is a 49-year-old man from Alaska. He was otherwise healthy but had been dealing with hypertension for many years. In addition, he has had hypokalemia (low potassium) and sleep apnea, which is very common in Conn’s syndrome.
In fact, he is so strong he used to be a competitor in the Iditarod (the world largest sled dog race in Alaska).
The patient had a left mini back scope adrenalectomy (MBSA) which took 26 minutes. The operation went well and he is doing great after surgery!
His next adventure is to ride his motorcycle from Alaska to the southern tip of Argentina.
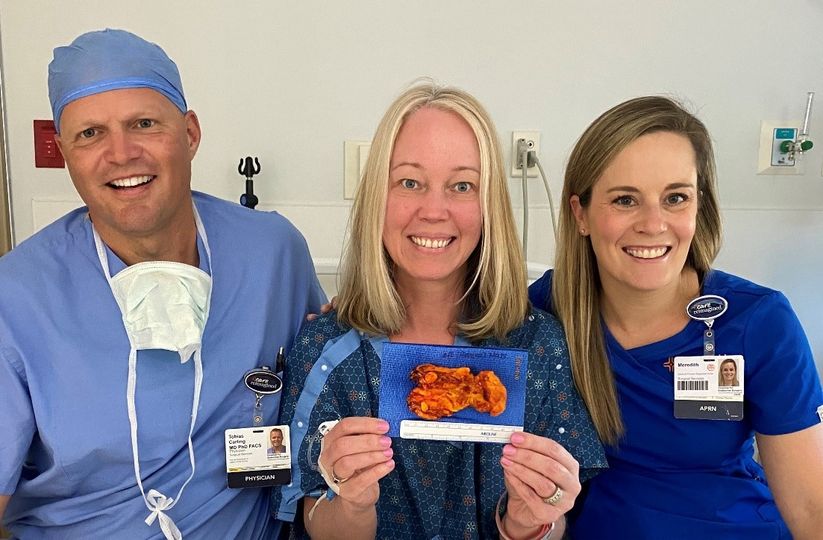
Interesting case of the week: Subclinical Cushing's syndrome in sweet lady
Many patients have subclinical Cushing’s syndrome due to an adrenal tumor, and only a fraction are properly diagnosed and treated. When you have subclinical Cushing’s syndrome, it’s due to a tumor of the adrenal gland that is producing too much cortisol. Toxic levels of cortisol can cause a lot of symptoms.
Today's patient is a 49-year-old female who had the following symptoms: heartburn, heart palpitations, muscle weakness, difficulty concentrating, difficulty with memory, irritability, easy bruising, thin skin, poor wound healing, stretch marks, anxiety, excessive hair loss, tremors, and panic attack symptoms.
Her labs all were consistent with subclinical Cushing’s syndrome. Her CT scan showed a 1.6 cm left adrenal mass.
This patient had a mini back scope adrenalectomy that took just 17 minutes. She did very well, and we anticipate the detrimental effects caused by cortisol overproduction will be reversed1
Here, the patient is pictured with Dr. Carling and Meredith LaRue (Dr. Carling’s APRN).
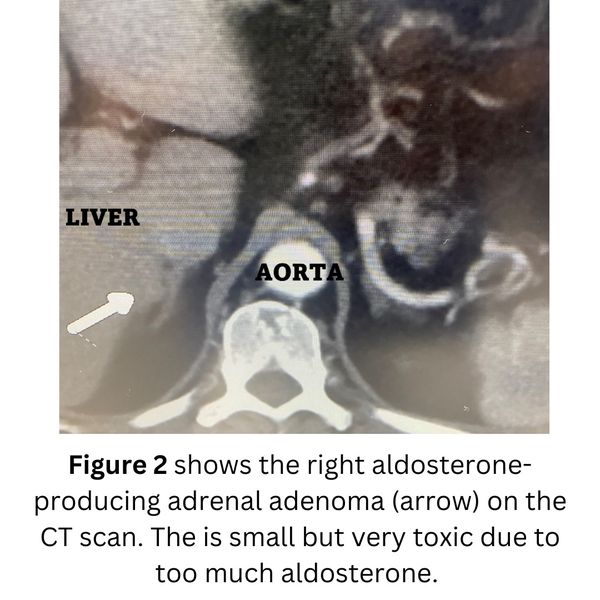
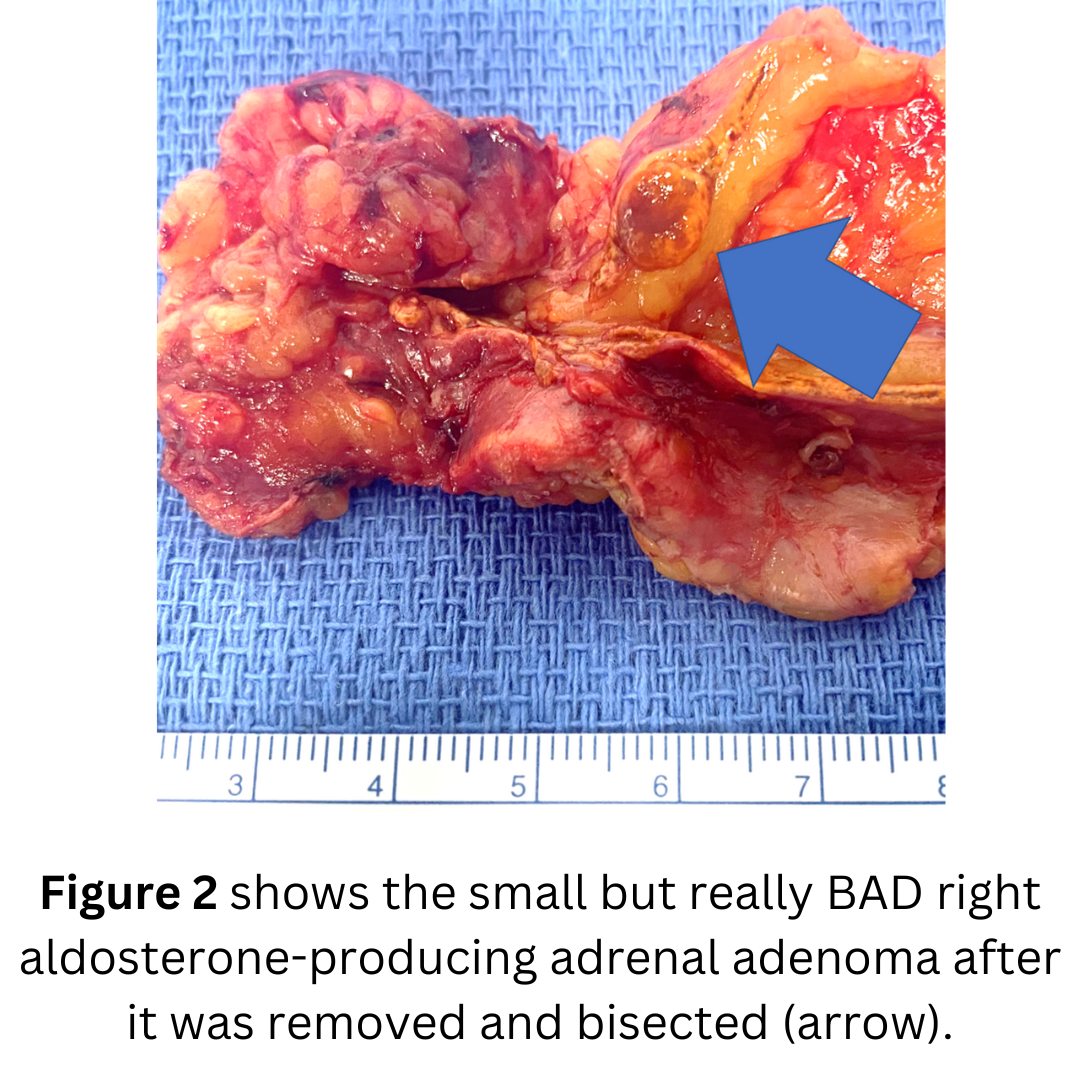
Interesting case of the week: Tiny aldosterone tumor causing huge problems in Michigan man
This case illustrates how a very small, but toxic aldosterone producing tumor can cause huge problems in an otherwise strong, and healthy man.
The patient is a 53-year-old Michigan man. He is otherwise healthy, but had for many years been dealing with hypertension. He also developed diabetes, hyperlipidemia (too high blood lipids; fat). His potassium was so low, he had to go to the emergency room. His potassium was as low as 2.7 - this is very bad!
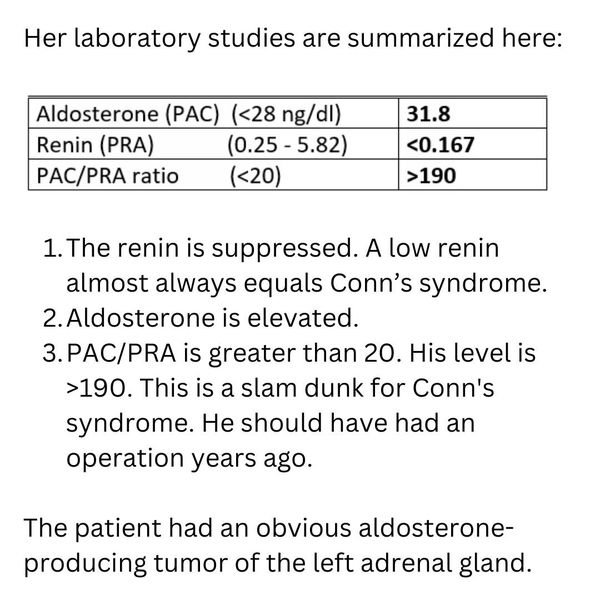
The patient's labs are shown in Figure 1. When you evaluate the labs for Conn’s syndrome (primary hyperaldosteronism) please note:
1) The renin is suppressed. A low renin almost always equals Conn’s syndrome (primary hyperaldosteronism)
2) Aldosterone is actually in the normal range in this man. Many patients with Conn’s syndrome (primary hyperaldosteronism) have aldosterone levels that are NORMAL. That is why you have to interpret the aldosterone and renin levels together!
3) PAC/PRA is greater than 20. His level is 175. This is SLAM DUNK ALDO. He should have had an operation years ago.
4) Potassium is very low.
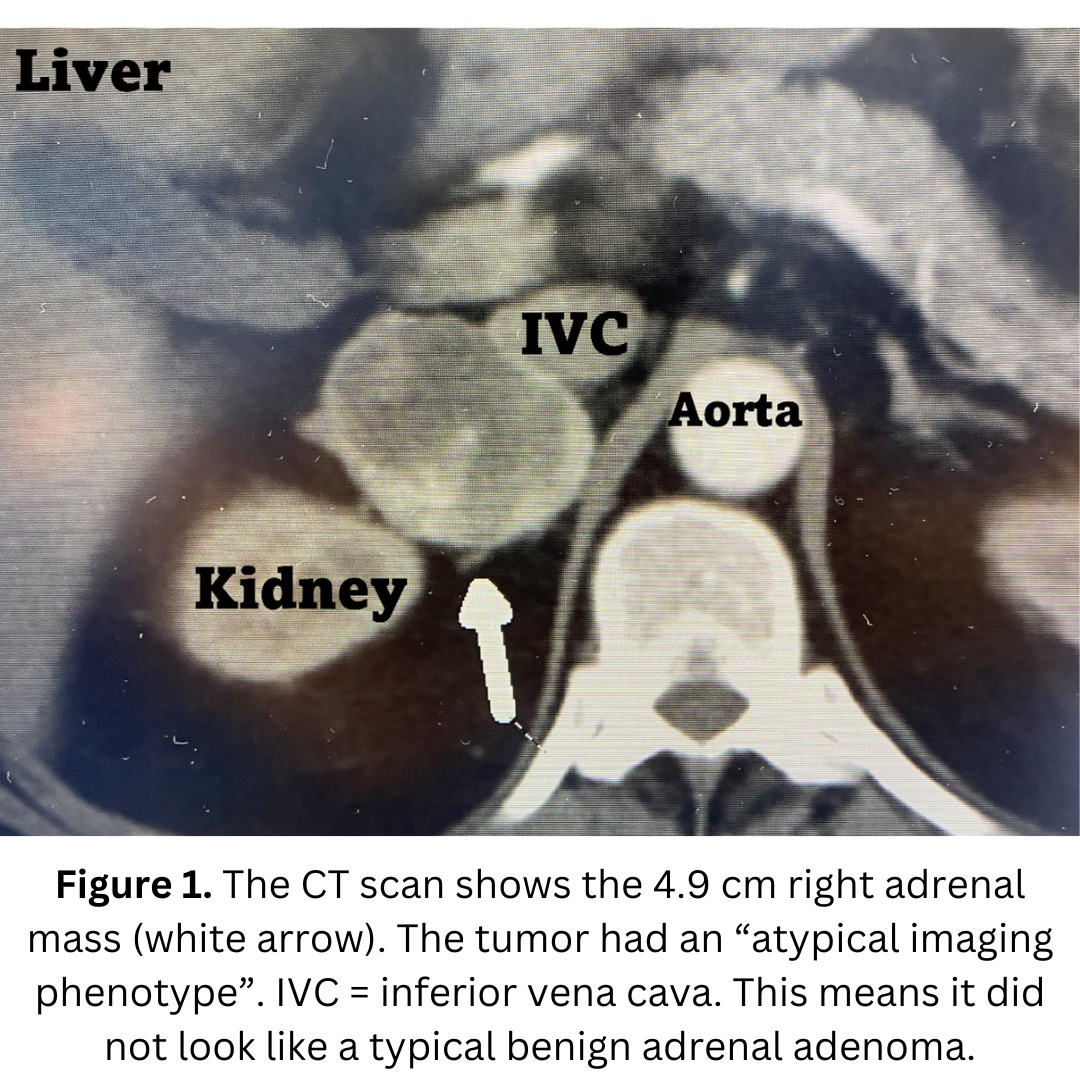
The patient had an obvious aldosterone-producing tumor of the right adrenal gland.
The patient had a right mini back scope adrenalectomy (MBSA) which took 21 minutes. The blood pressure normalized very quickly, and he will do tremendously well after surgery.
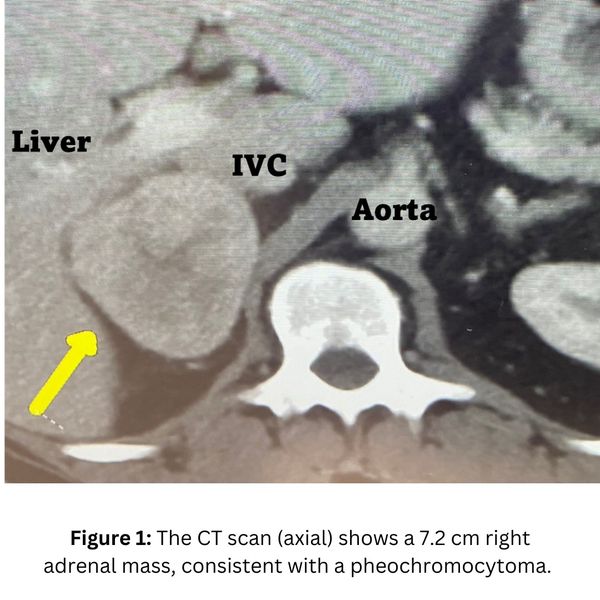
Interesting case of the week: Large pheo in Georgia man
Today's patient is a 51-year-old man from Georgia. He underwent a CT scan which revealed a large right adrenal tumor, greater than 7 cm, or about the size of an orange. In retrospect, he has suffered many years from hypertension, heart palpitations, excessive sweating, anxiety, dizziness and diabetes. These are all symptoms of pheochromocytoma.
Even though the tumor was large, he was a great candidate for the Mini Back Scope Adrenalectomy (MBSA).
The patient did tremendously well. His blood pressure was cured in the operating room. He was up walking around the day of surgery, and he will bounce back quickly. His symptoms are already gone.
Interesting case of the week: Adrenal tumors on both sides in Conn's syndrome
Primary hyperaldosteronism, or Conn’s syndrome, affects patients of all ages, but is especially common in young women. The good news is that when operated on, young women have close to a 100% cure rate of their primary hyperaldosteronism.
Today's patient is a 32-year-old woman from Virginia, otherwise healthy and slender. She was a textbook case of Conn’s syndrome, but like many patients, it took years to arrive at the correct diagnosis. For several years, she had been suffering from hypertension, hypokalemia (low potassium; this is bad) and many other classic symptoms.
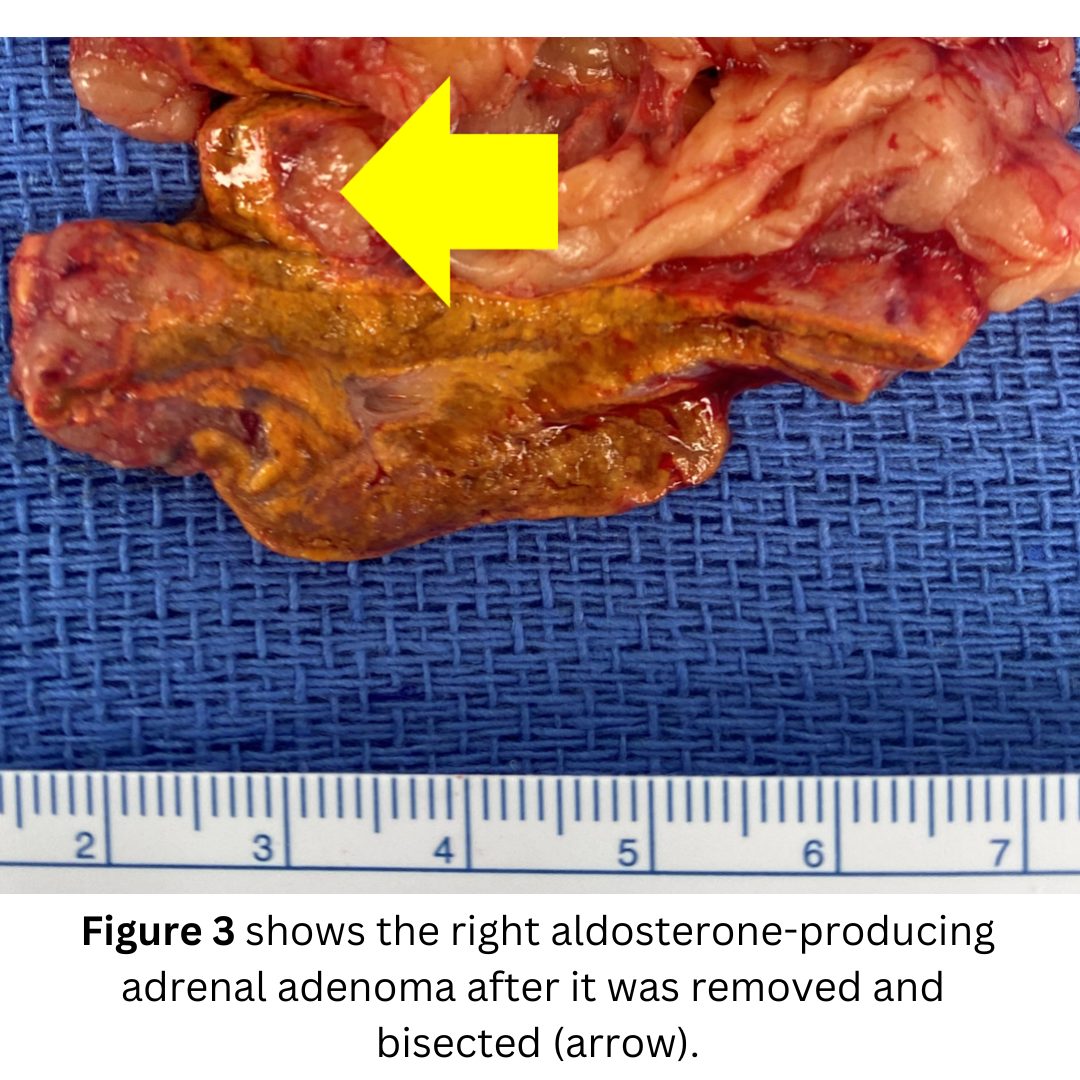
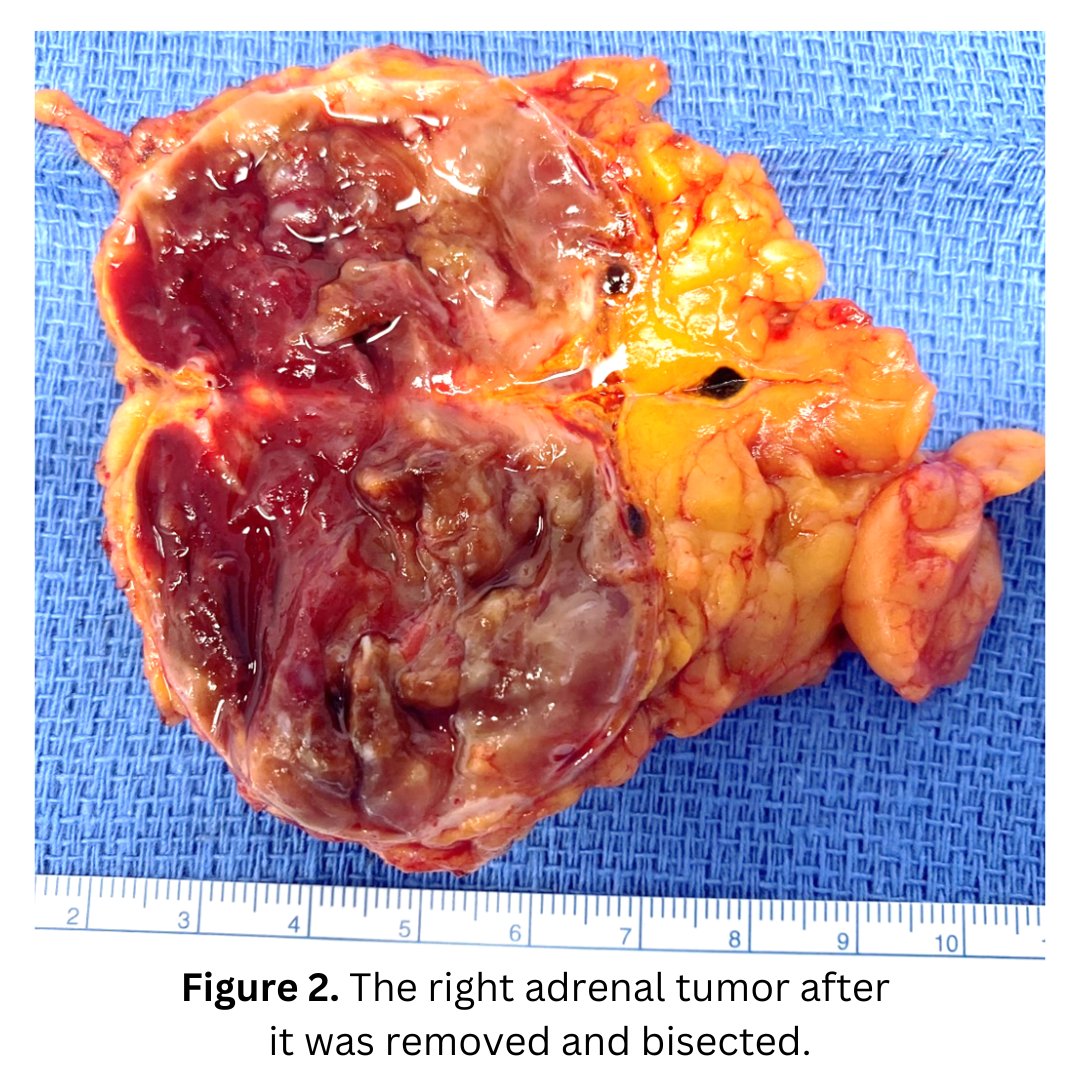
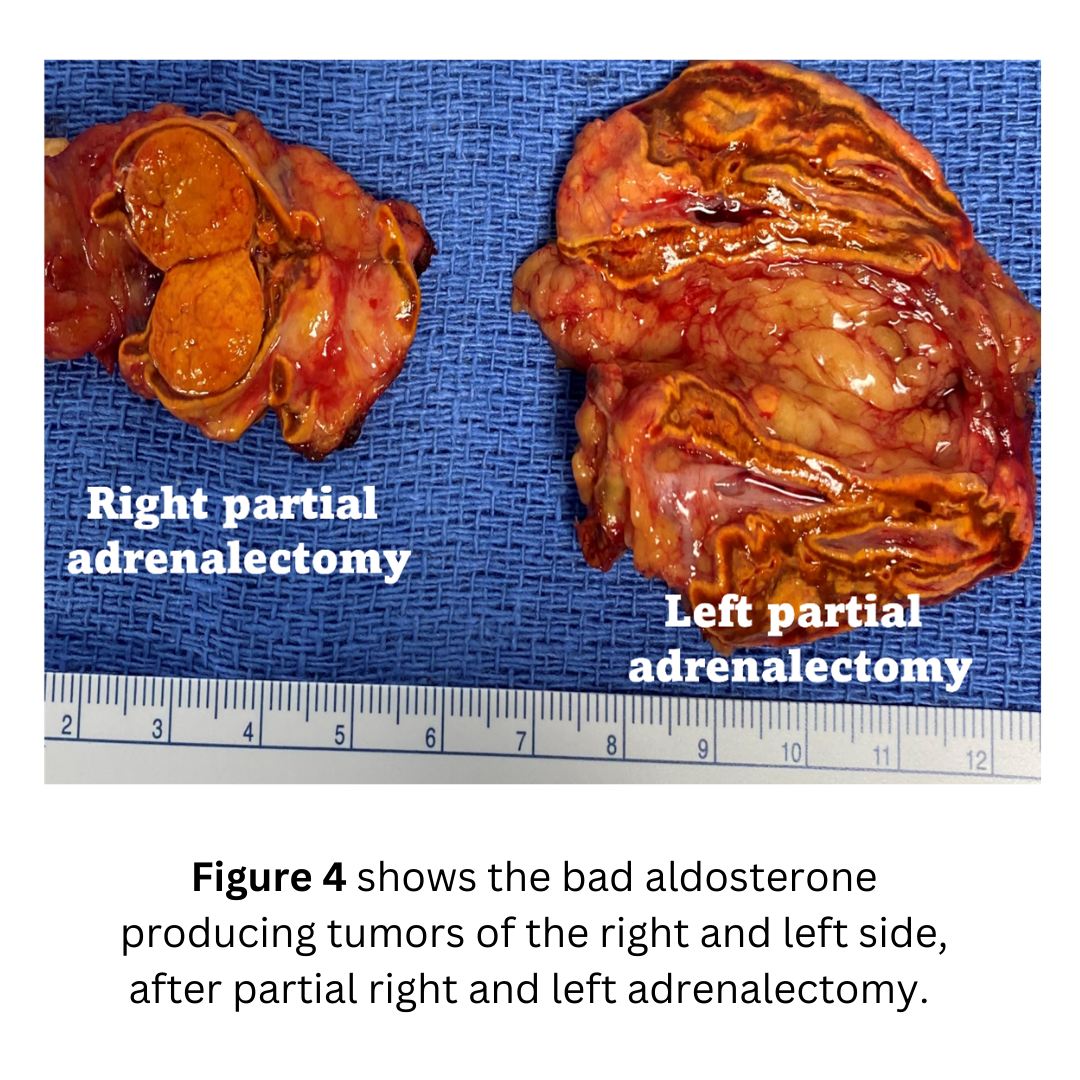
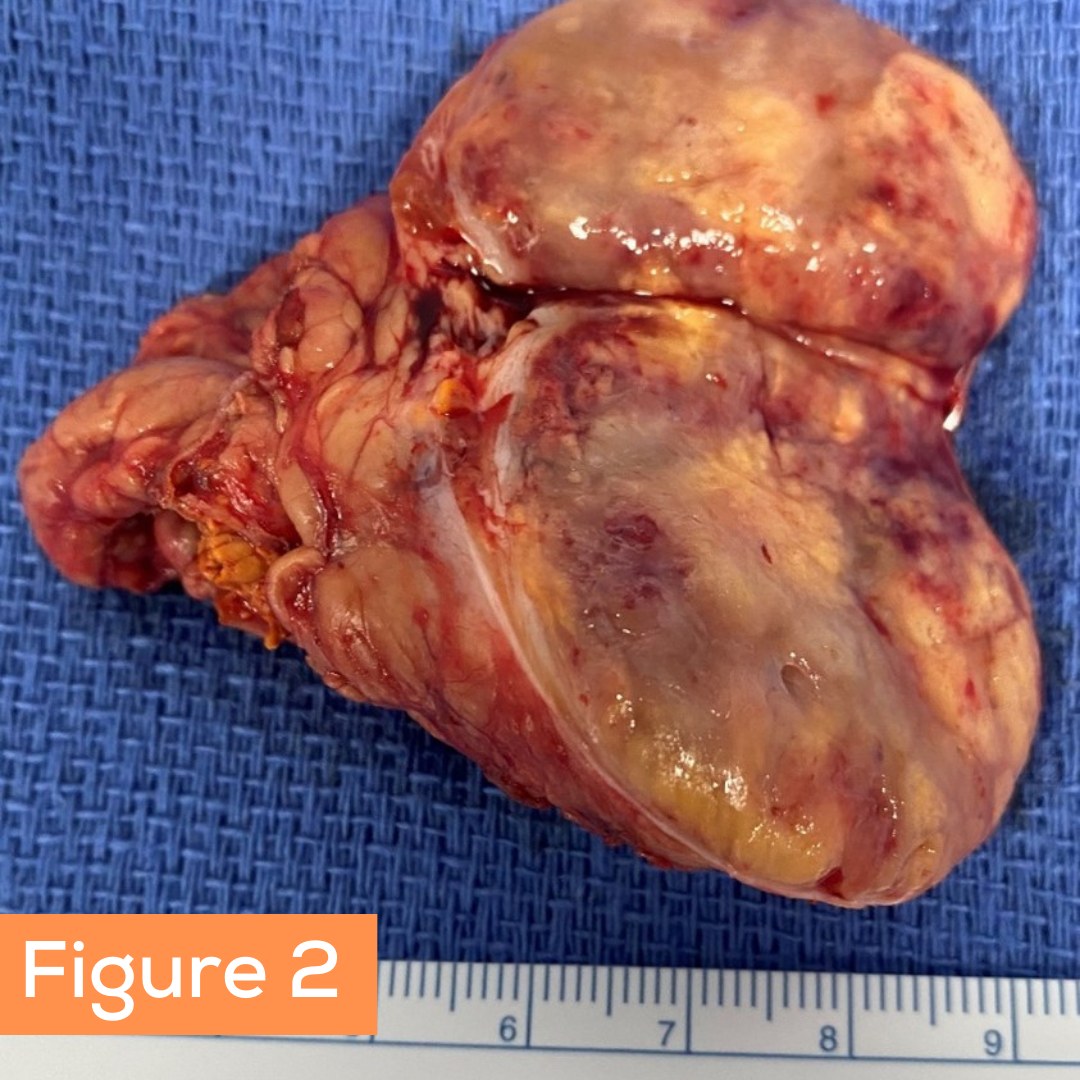
Her laboratory studies are summarized in Figure 1 and her scans are pictures in Figures 2 and 3. Her scans showed she had a tumor on each adrenal.
She contacted us for help. Dr. Carling reviewed her case and discussed all the options with her. The patient opted for a bilateral adrenalectomy via MBSA, preserving the prefect amount of tissue so that she would not need to take steroids.
The patient's operation took about 20 minutes. Her blood pressure normalized very quickly, and she will do tremendously well. Her cosyntropin stimulation test was completely normal. This means her remnant adrenal tissue works perfectly and she will not have to take steroids.
Interesting case of the week: Pheochromocytoma incidentally found
The symptoms of adrenal pheochromocytoma can be variable, and are often missed by doctors for years. The top 5 symptoms of pheochromocytoma are high blood pressure, headaches, racing heartbeat, sweating and anxiety.
All symptoms of a pheochromocytoma are due to the very toxic effects of too much adrenaline hormones (catecholamines).
Today's patient is a 76-year-old local woman from the Villages in Florida. She had a history of high blood pressure as well as previous heart attack, and atrial fibrillation. These are common manifestations of the toxic effects of adrenaline hormones over years and decades.
The patient had a very swift 19-minute mini back scope adrenalectomy (MBSA).
The patient did fabulously well and resumed all her activities within a week after the operation. She will be protected from further high blood pressure, heart attacks and stroke!
Interesting Case of the Week: Conn's syndrome patient from New Jersey
This week's patient is a 44-year-old lady from New Jersey. She was a textbook case of Conn’s syndrome (primary hyperaldosteronism). For several years, she had been suffering from hypertension and hypokalemia (low potassium; this is bad).
She had a CT scan which showed an obvious tumor on the right adrenal gland.
This tumor had very low Hounsfield units (HU), which in a young woman means that they almost always have a somatic (meaning acquired, not inherited) KCNJ5 mutation within the tumor.
Dr. Carling published the most important science on the molecular pathogenesis of primary hyperaldosteronism and Conn’s syndrome. His research has helped us understand this disease much better and leads to personalized and individualized treatment.
This means this patient could have moved straight to adrenal surgery without having adrenal vein sampling (AVS).
The patient’s doctors in New Jersey were not aware of these most recent scientific discoveries, and the patient was thus referred for adrenal vein sampling (AVS). Not surprisingly, this demonstrated 29 times more aldosterone production from the right adrenal versus the left. It's not the end of the world that the patient had an unnecessary procedure, however, with new data we can be more precise and spare unnecessary tests and procedures.
The patient had a right mini back scope adrenalectomy (MBSA) that took 17 minutes. She is doing great!
Interesting case of the week: Subclinical Cushing’s in a local woman
Although many patients fly in for their adrenal surgery from all 50 states and internationally, we love our Florida patients, too!
Today's patient is a 65-year-old woman from Florida. She was suffering from hypertension, heart palpitations, leg and arm cramps, muscle weakness, difficulty concentrating, difficulty with memory, irritability and crankiness, easy bruising, thin skin, stretch marks (especially on the lower abdomen and upper thighs), anxiety, pre-diabetes and diabetes mellitus, excessive hair loss, hypokalemia, sleep apnea, weight gain with central obesity, tremor, excessive sweating, and panic attack symptoms.
Her laboratory tests showed that her ACTH level was on the low side, but her low dose dexamethasone suppression test (LDDST) was elevated. This proves that her Cushing’s syndrome arose from an adrenal source.
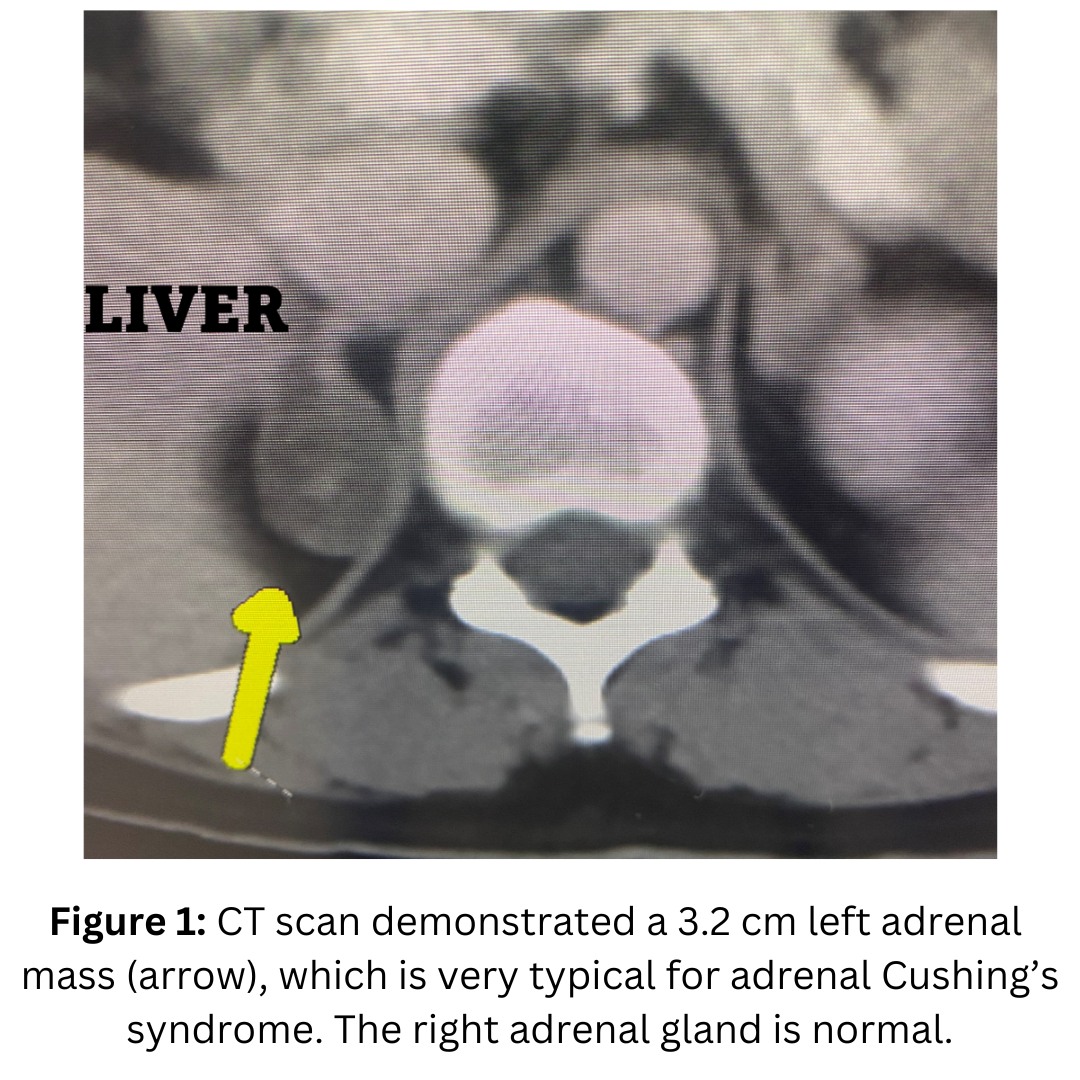
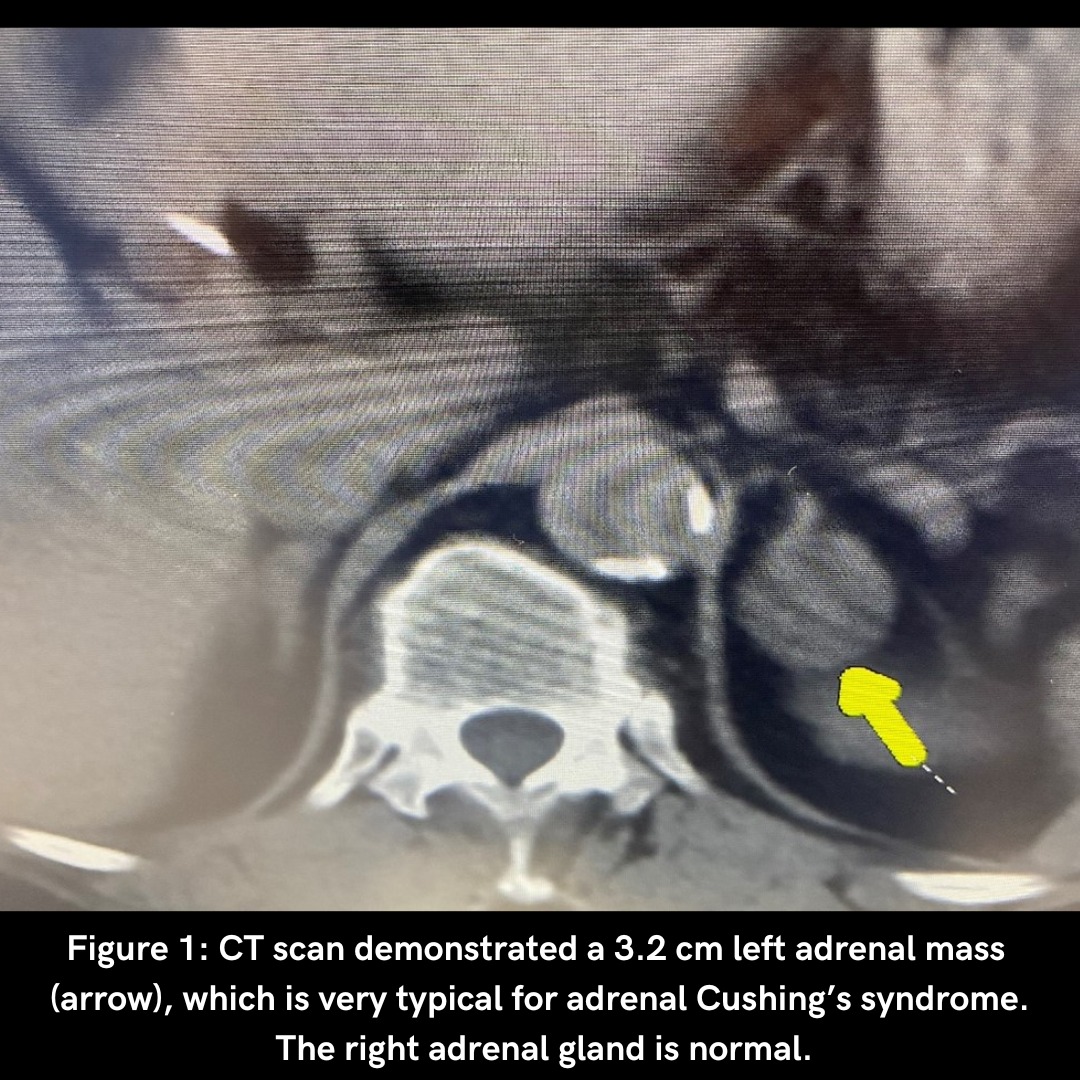
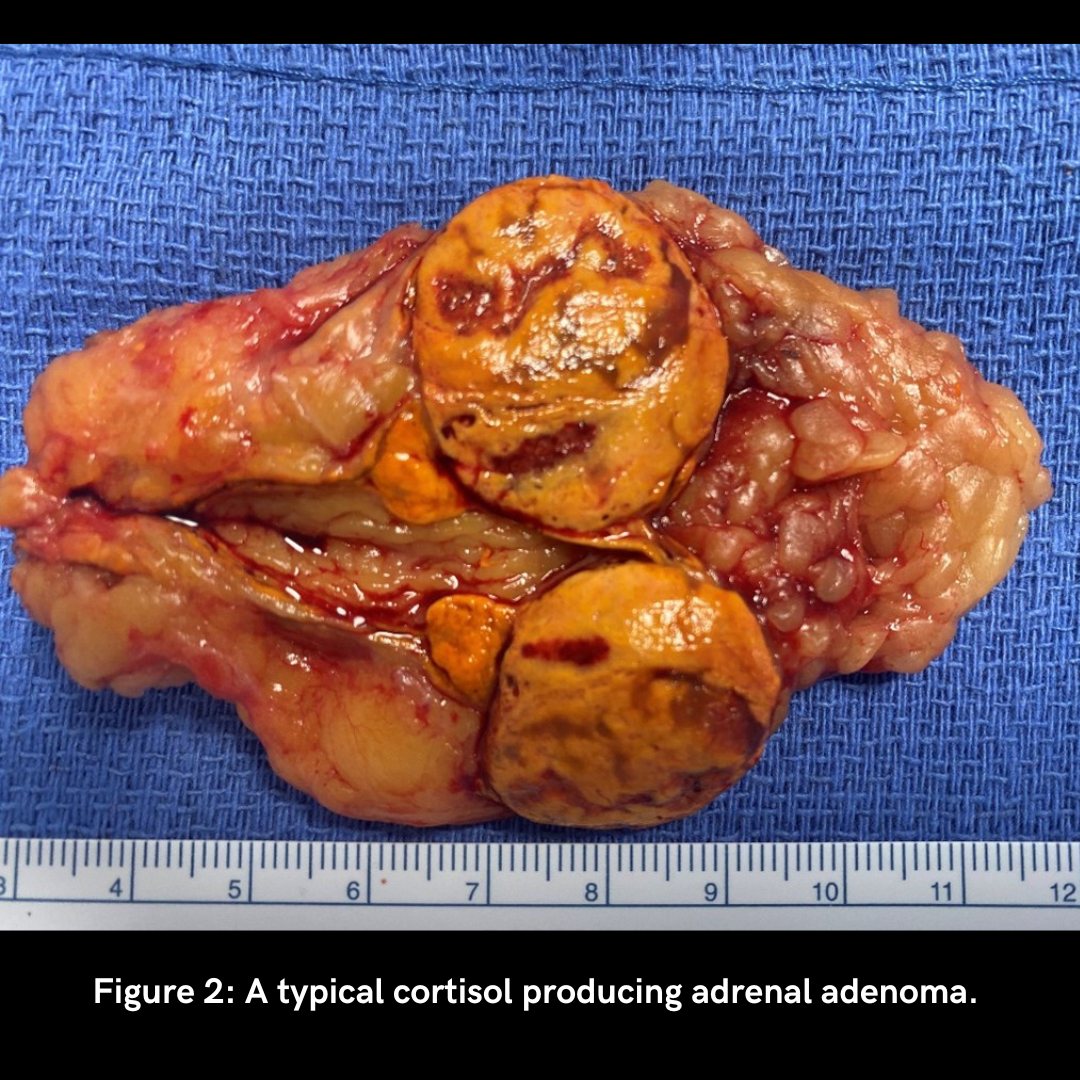
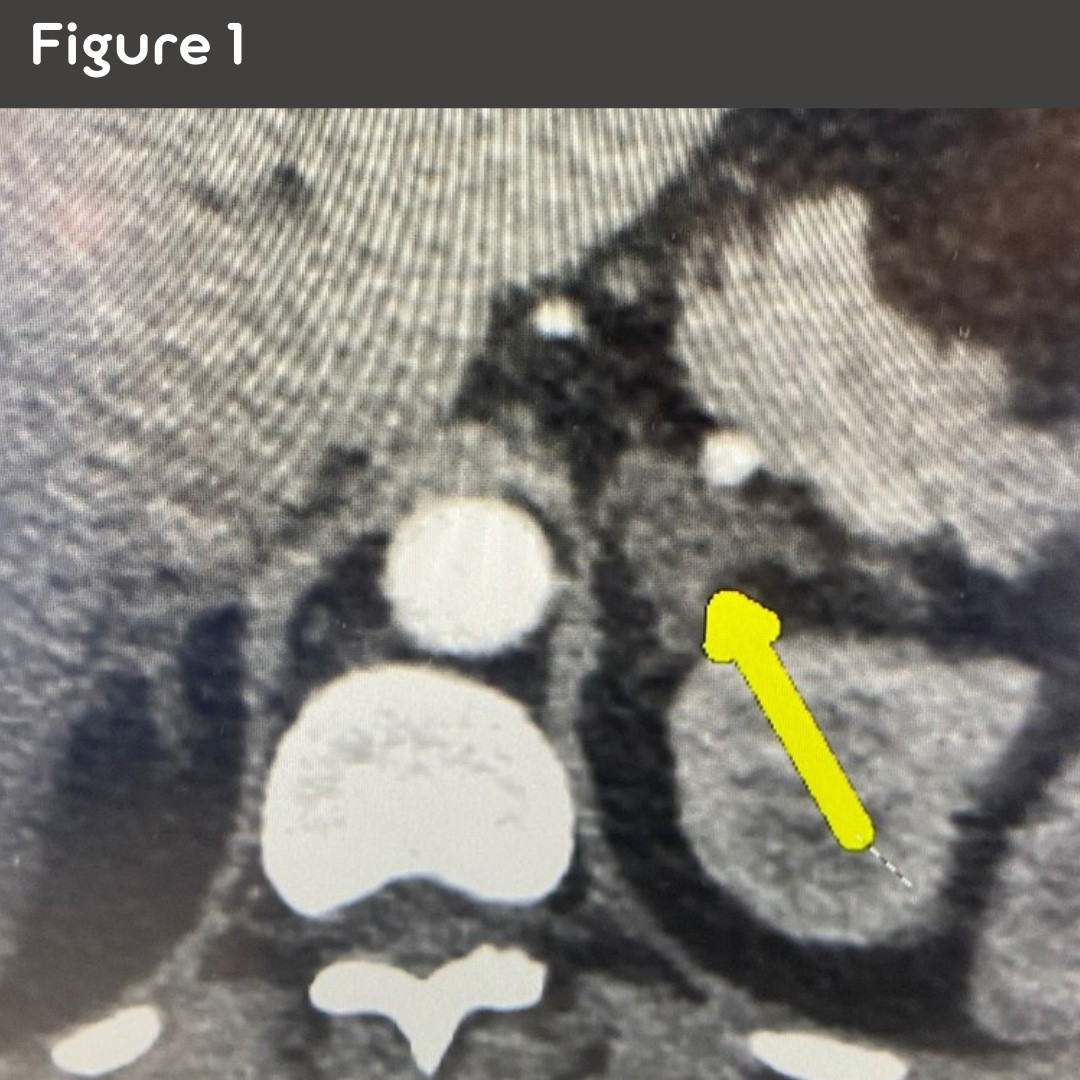
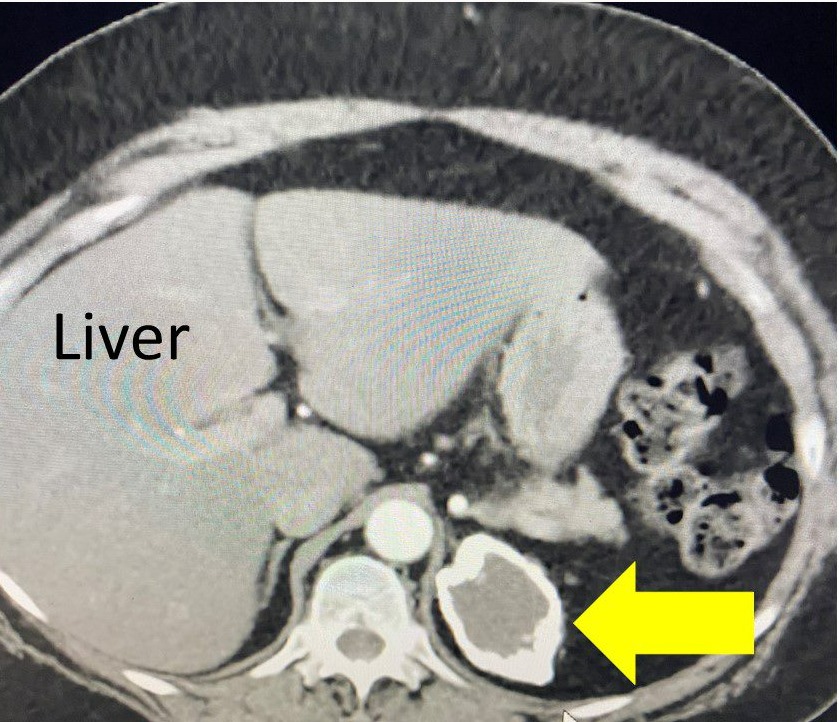
Figure 1. CT scan demonstrated a 3.2 cm left adrenal mass (arrow), which is very typical for adrenal Cushing’s syndrome. The right adrenal gland is normal
The patient underwent an 18-minute Mini Back Scope Adrenalectomy (MBSA) on the left side. Very soon, the patient felt much better!
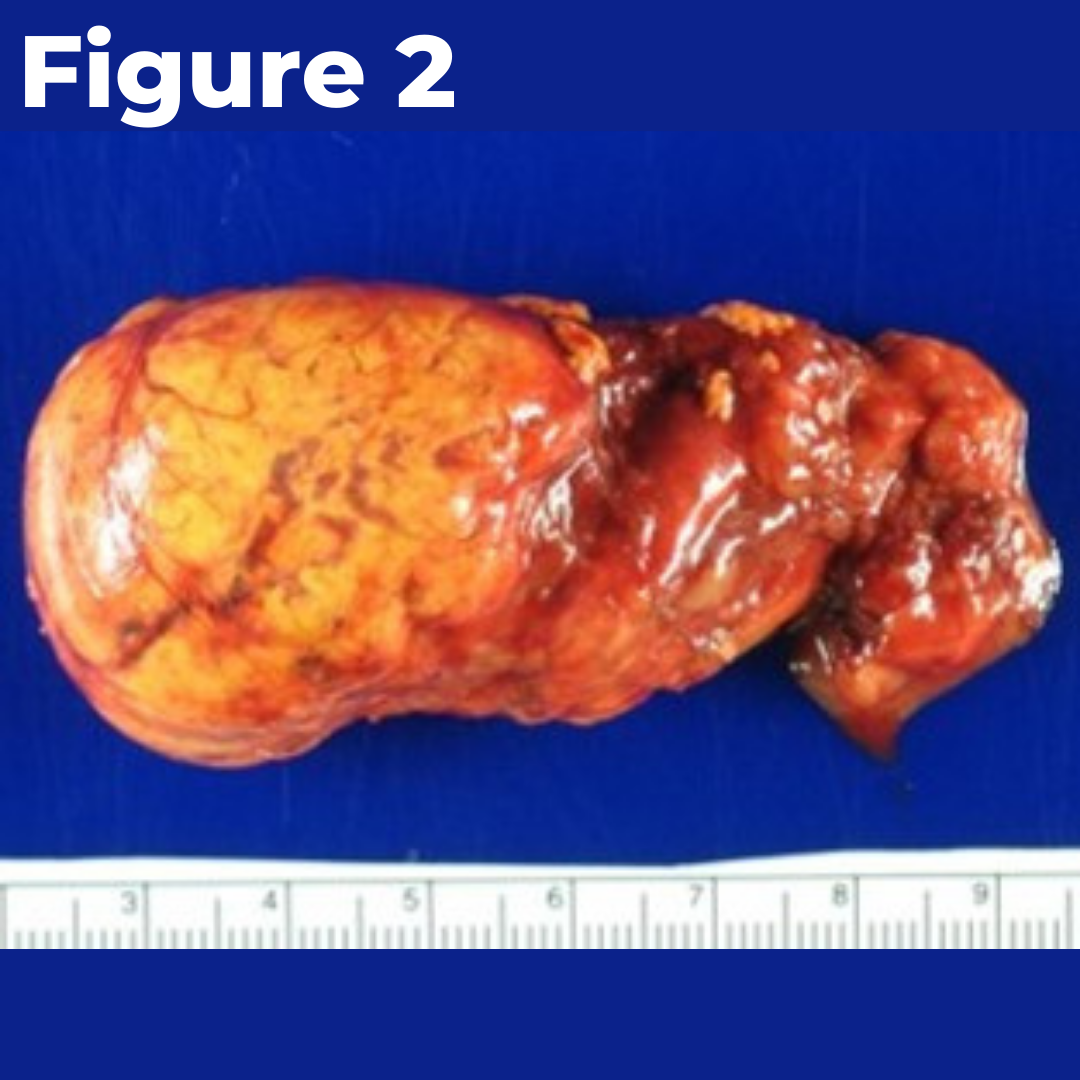
Figure 2 demonstrates a typical cortisol producing adrenal adenoma.
Interesting case of the week: A New Yorker with Adrenal Metastasis
This week's patient is a 67-year-old man from upstate New York. Two years ago, he was diagnosed with renal cell cancer and underwent a radical left nephrectomy and left adrenalectomy.
Initially he was doing very well after his operation. He required some strong chemotherapy treatment which caused hypophysitis (inflammation of pituitary) and pituitary failure which required him to take Hydrocortisone.
A follow up scan one year after the kidney operation demonstrated a right adrenal mass measuring 1.2 cm. Over the next several months, the tumor on the right adrenal gland continued to grow. Fortunately, there was no other evidence of cancer anywhere else.
He contacted the Carling Adrenal Center to see if it would be feasible to remove the right adrenal metastasis (originating from the kidney cancer) via the Mini Back Scope Adrenalectomy (MBSA) procedure.
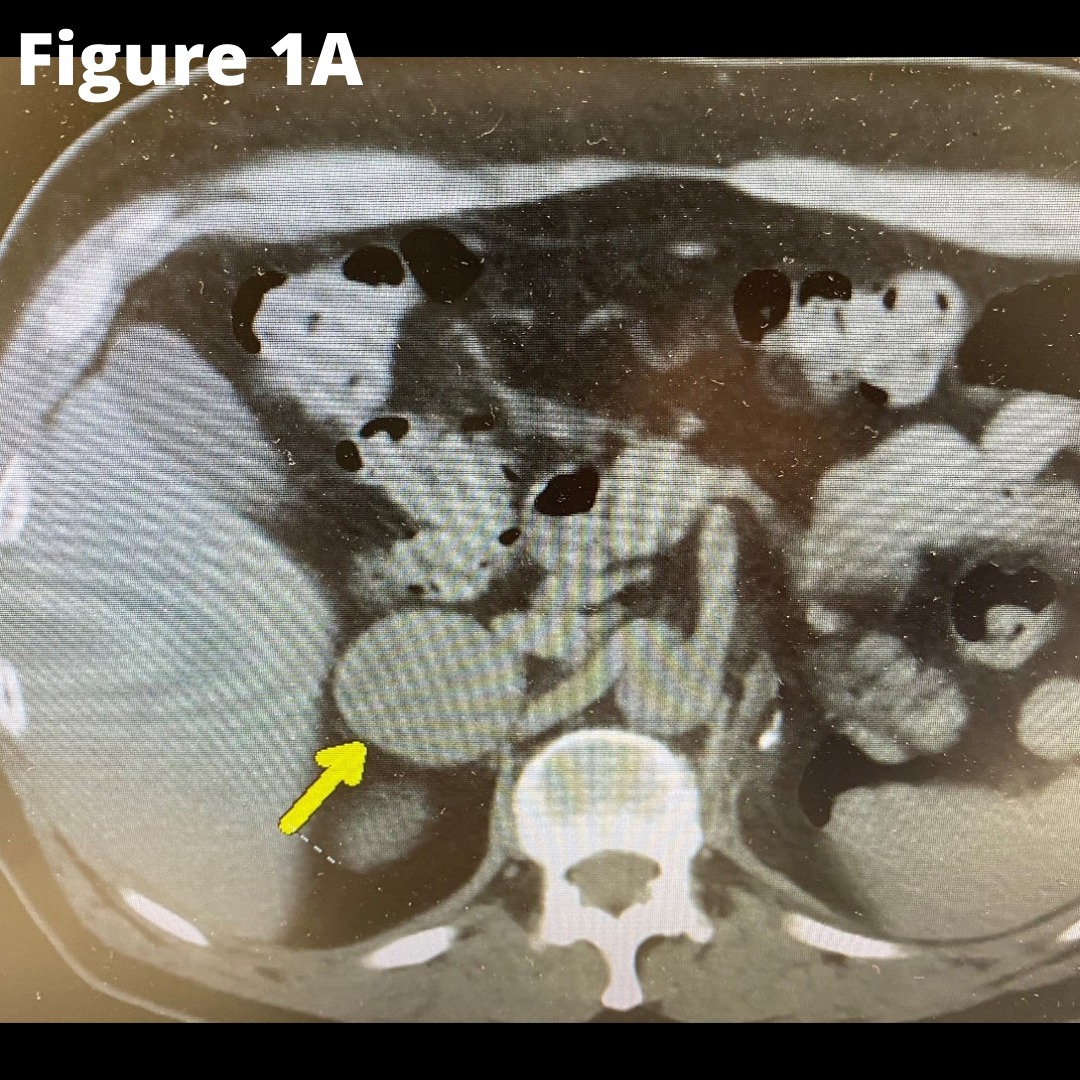
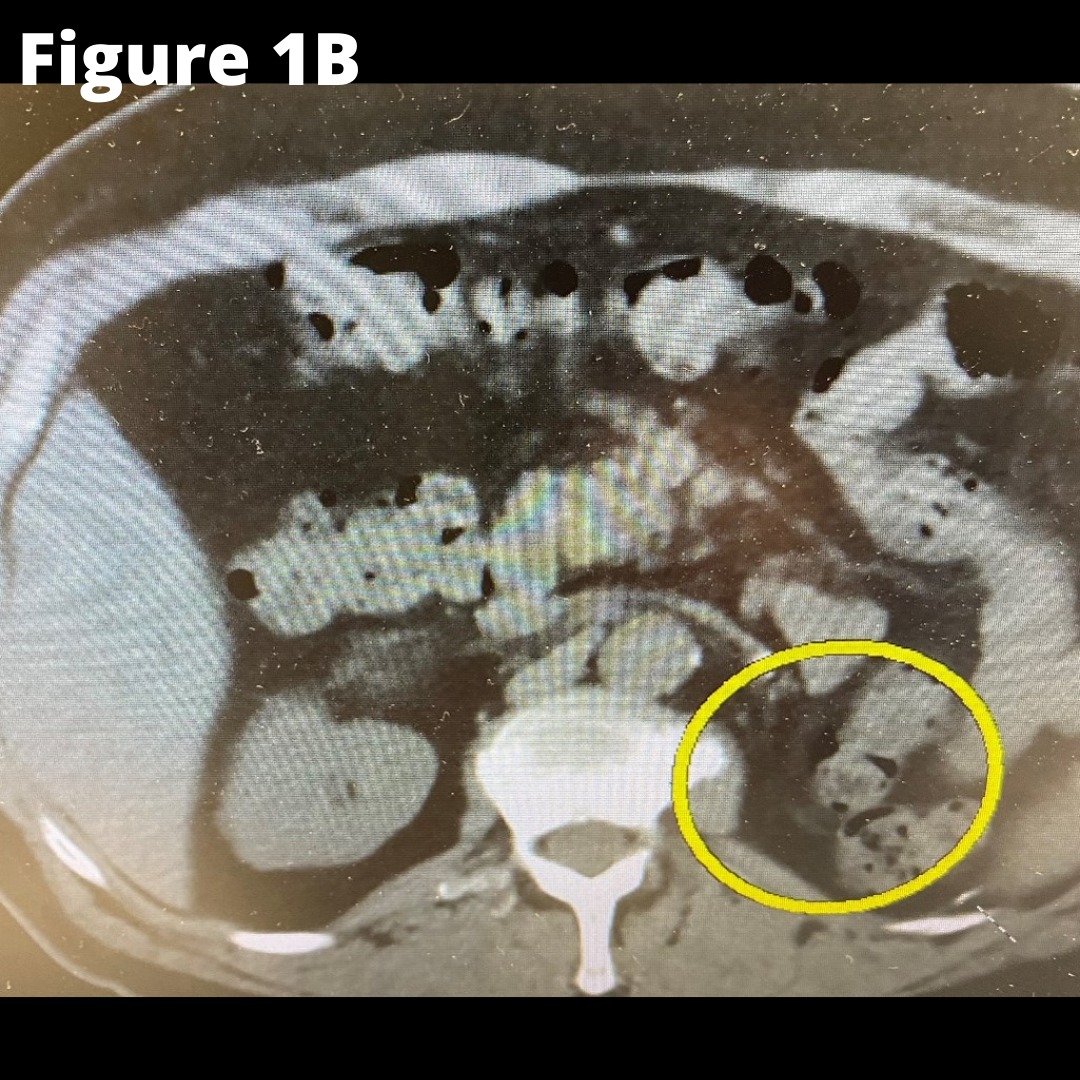
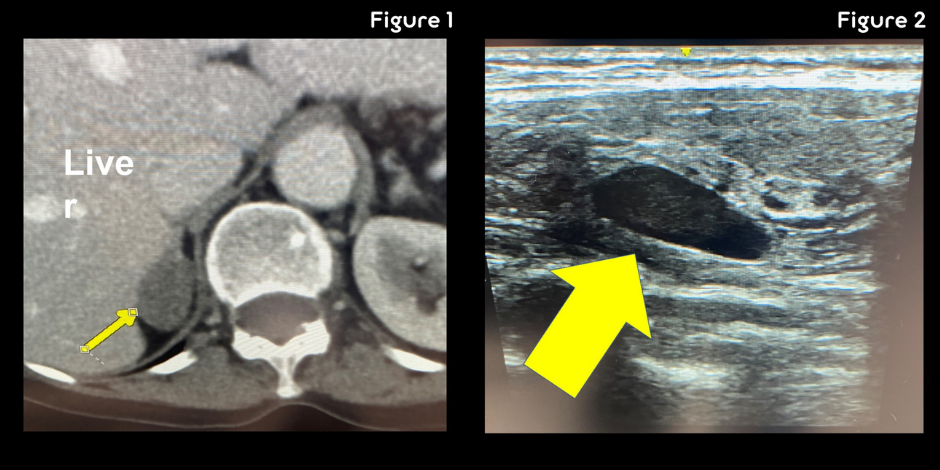
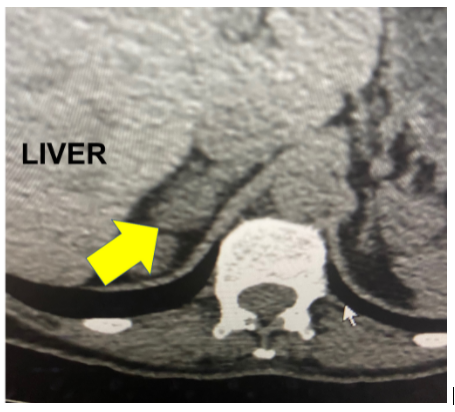
Figure 1A shows the CT scan. The yellow arrow indicate the right adrenal mass. Figure 1B shows the absent left kidney and absent left adrenal that was removed during the surgery for kidney cancer.
This patient underwent the MBSA procedure successfully. Sometimes adrenal metastasis can be very inflamed and stuck to surrounding structures (making the operation slightly more complex), but this gentleman’s tumor came off the inferior vena cava (IVC) quite nicely.
He flew back home shortly thereafter and will continue to be closely monitored by his local oncologist.
Interesting case of the week: A Minnesota Mayor with bilateral Conn's syndrome
As the pandemic is waning, we are seeing an uptick in international patients again. Today's case is about a 56-year-old man from Canada. For several years, he suffered from hypertension and hypokalemia (low potassium). More recently, he began experiencing symptoms like muscle cramps, difficulty with memory and concentration, and anxiety.
The patient is a 44-year-old lady from Minnesota. She’s been plagued with low potassium and high blood pressure for many years. She was already on three blood pressure medications, and she was only 44 years old. Her symptoms included heart palpitations, cramps, muscle weakness, difficulty concentrating, mood changes, anxiety, and more.
Her laboratory work-up showed that her potassium was consistently low. Her aldosterone level was very high at 61 and her plasma renin activity (PRA) was low. This proved that she had primary hyperaldosteronism (Conn’s syndrome).
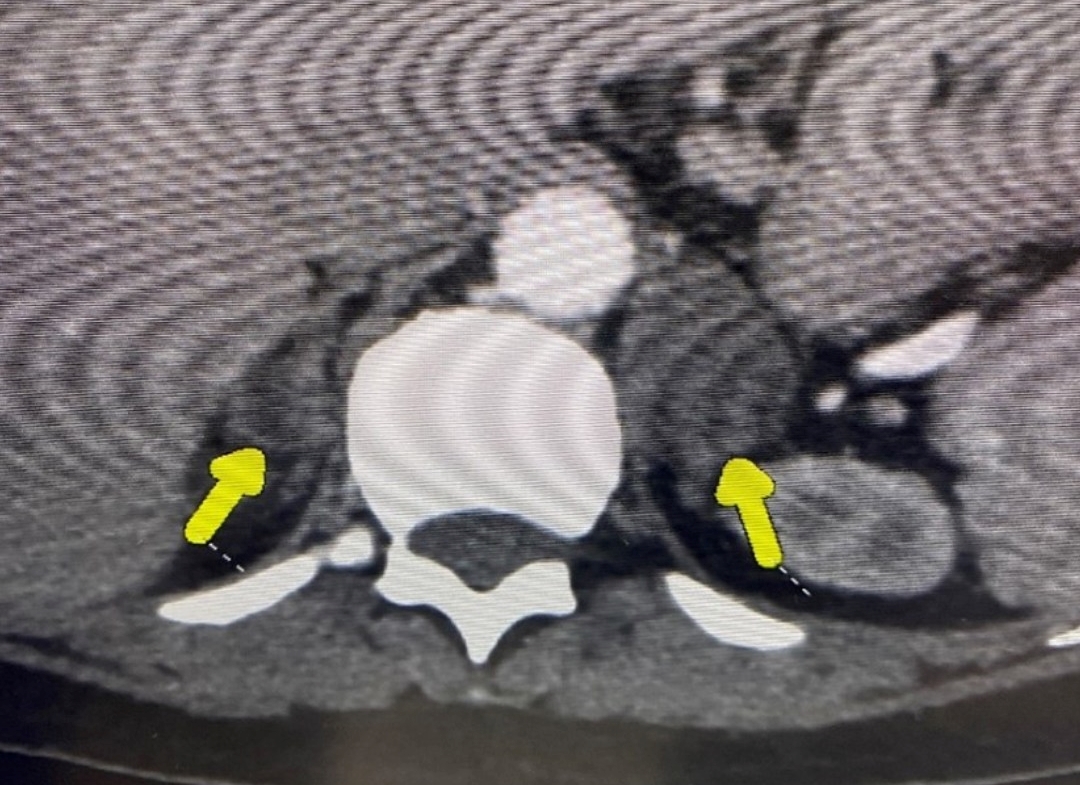
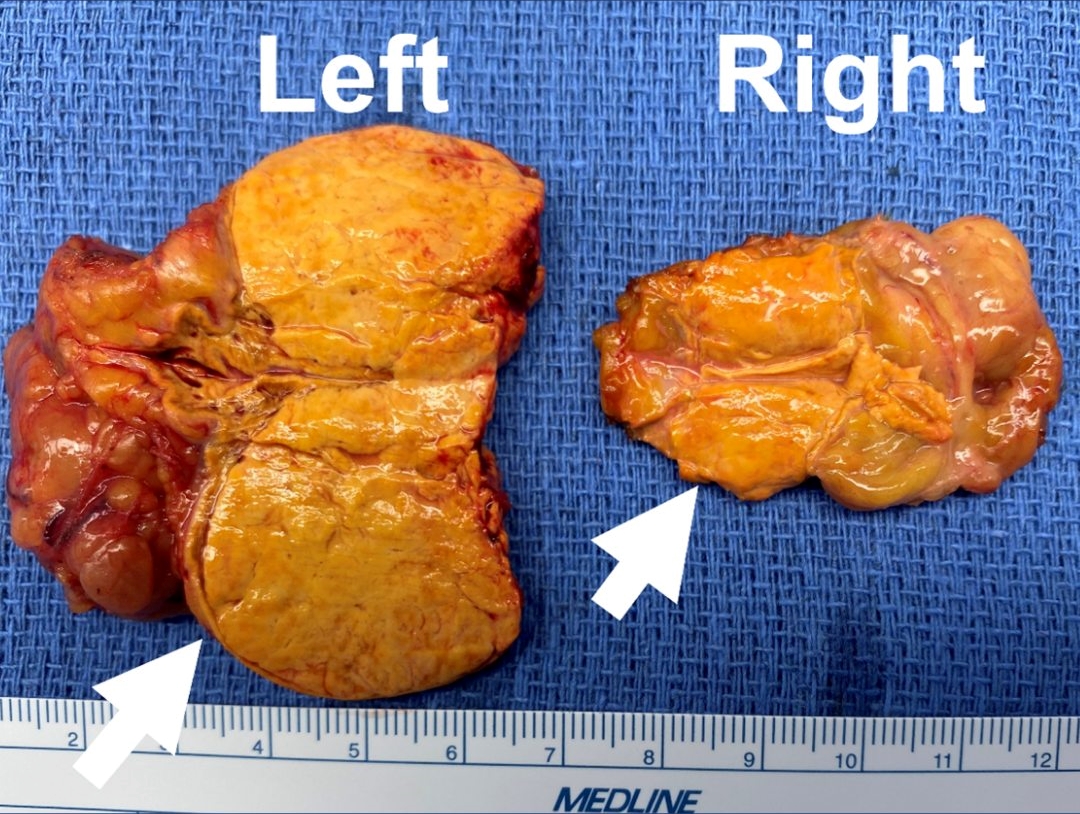
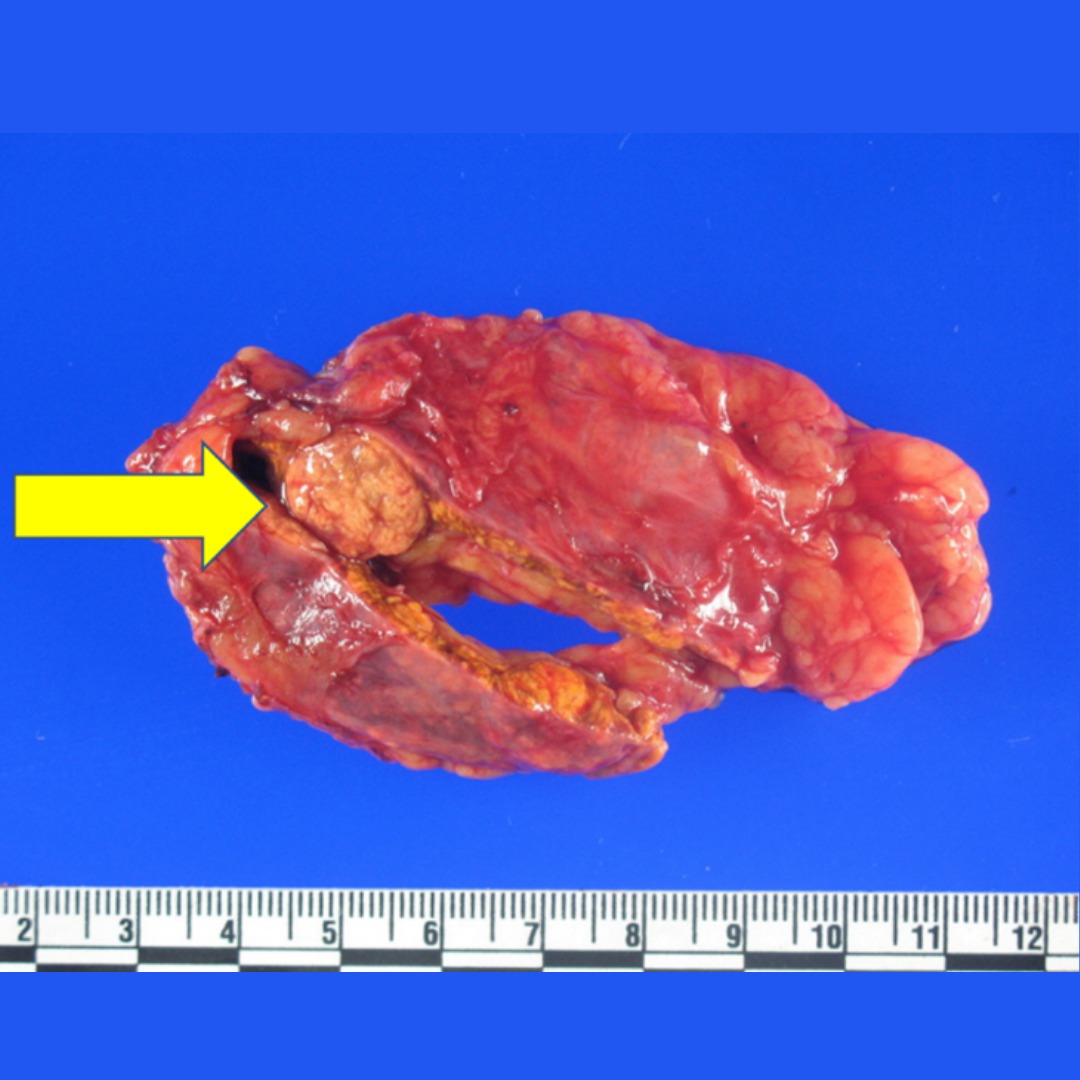
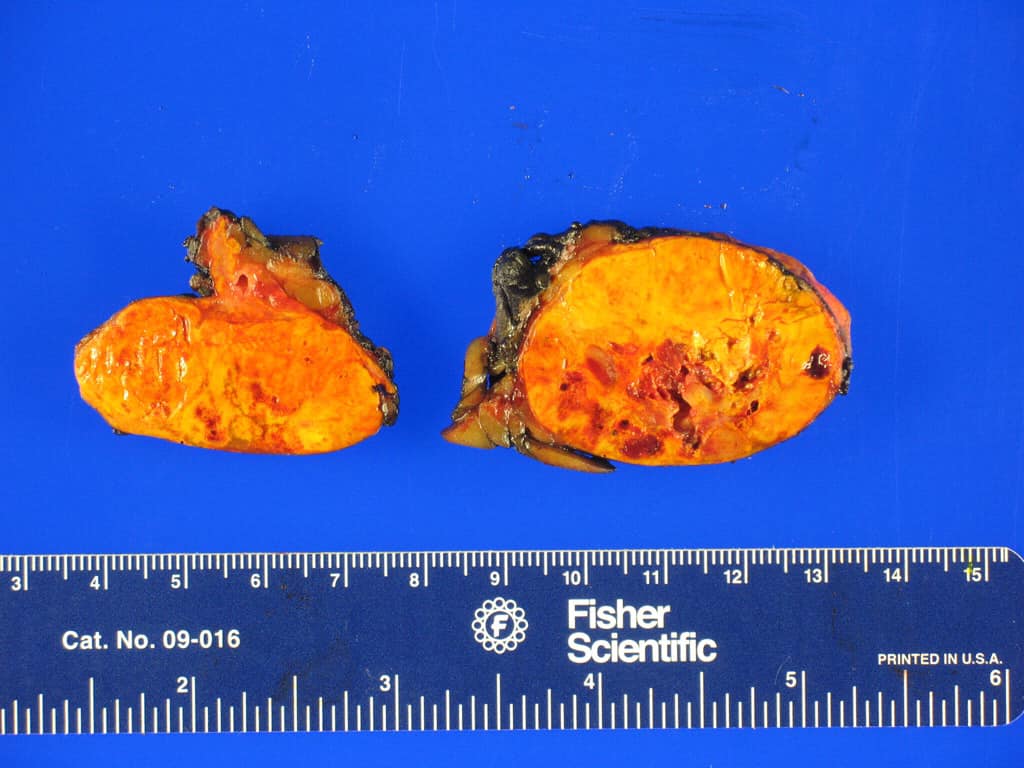
She had a CT scan which revealed she had tumors both on the left side and the right side, leaving her doctors stumped. Figure shows the smaller adrenal tumor on the right side (shorter arrow; 1.7 cm) and the larger tumor on the left side (2.7 cm).
She didn't know what to do and decided to contact the Carling Adrenal Center. We talked through the options, including adrenal vein sampling. Because this is a time consuming procedure and the success rate is not 100%, the patient asked “Can’t you just remove the tumors, and do a partial adrenalectomy on both sides?” Ultimately, this is what the patient wanted. She did not want more diagnostic procedures. She wanted curative surgery.
We performed a bilateral partial adrenalectomy via the mini back scope adrenalectomy (MBSA) approach. Each operation took about 15 minutes.
Figure 2: Pathology showing the smaller adrenal tumor on the right side (shorter arrow; 1.7 cm) and the larger tumor on the left side (2.7 cm). The tumors were consistent with aldosterone-producing adrenal adenomas.
The patient did tremendously well after surgery. Her blood pressure improved dramatically over the next 24 hours and continues to improve. There's a good chance she will be able to come off her blood pressure medications altogether. The operation will protect her against future heart arrhythmias, heart attacks and stroke.
And yes, we did check her adrenal function (via a cosyntropin (ACTH) stimulation test) at 4 am the next morning, and it was perfect. This proves that she has perfectly normal adrenal function, and does not need to take steroids such as hydrocortisone and prednisone.

Interesting case of the week: A Michigan artist with a grateful heart and Subclinical Cushing’s syndrome
The patient is a 58-year-old artist from Michigan with subclinical Cushing’s syndrome. The patient's signs and symptoms included high blood pressure, heartburn, heart palpitation, muscle weakness, neurocognitive symptoms, central obesity, anxiety, hair loss and weight gain.
Her laboratory tests showed that her ACTH level was on the low side but her low dose dexamethasone suppression test (LDDST) as well as 24-hour urine free cortisol (UFC) were elevated. This proves that her Cushing’s syndrome arose from an adrenal source.
Her CT scan initially had caused some confusion by her doctors because she had one tumor on the right side measuring 1.8 cm and one tumor on the left side measuring 1.3 cm. When Dr. Carling reviewed the scan, it was obvious that the tumor on the left side was adrenal myelolipoma and was not contributing to her Cushing’s syndrome at all. The disease and high cortisol came from the tumor on the right side.
Thus, she underwent a 23-minute Mini Back Scope Adrenalectomy (MBSA) on the right side. The patient felt much better after surgery. She was so thrilled that she even donated a beautiful painting to Dr. Carling and the team at the Carling Adrenal Center. In the painting, you'll see the outline of a heart and she named the piece “a grateful heart”.
Here at the Carling Adrenal Center, we are very thankful and have grateful hearts for all the patients traveling to us from all 50 US states and internationally every single week. We love taking care of our patients, learning their stories, and sharing in their lives.
Interesting case of the week: Conn's syndrome patient from Canada turns to Dr. Carling
As the pandemic is waning, we are seeing an uptick in international patients again. Today's case is about a 56-year-old man from Canada. For several years, he suffered from hypertension and hypokalemia (low potassium). More recently, he began experiencing symptoms like muscle cramps, difficulty with memory and concentration, and anxiety.
His symptoms were very typical for Conn’s syndrome (primary hyperaldosteronism), though his diagnosis took a long time.
Eventually he had the correct tests done, revealing his aldosterone was very high while his renin was suppressed proving that he had Conn’s syndrome.
Our patient lives in British Columbia and contacted us because he was getting the runaround within the Canadian healthcare system. He saw the most experienced adrenal surgeon in Canada, and learned he only performs #adrenalsurgery through the belly (you DO NOT want the adrenal tumor removed through the belly).
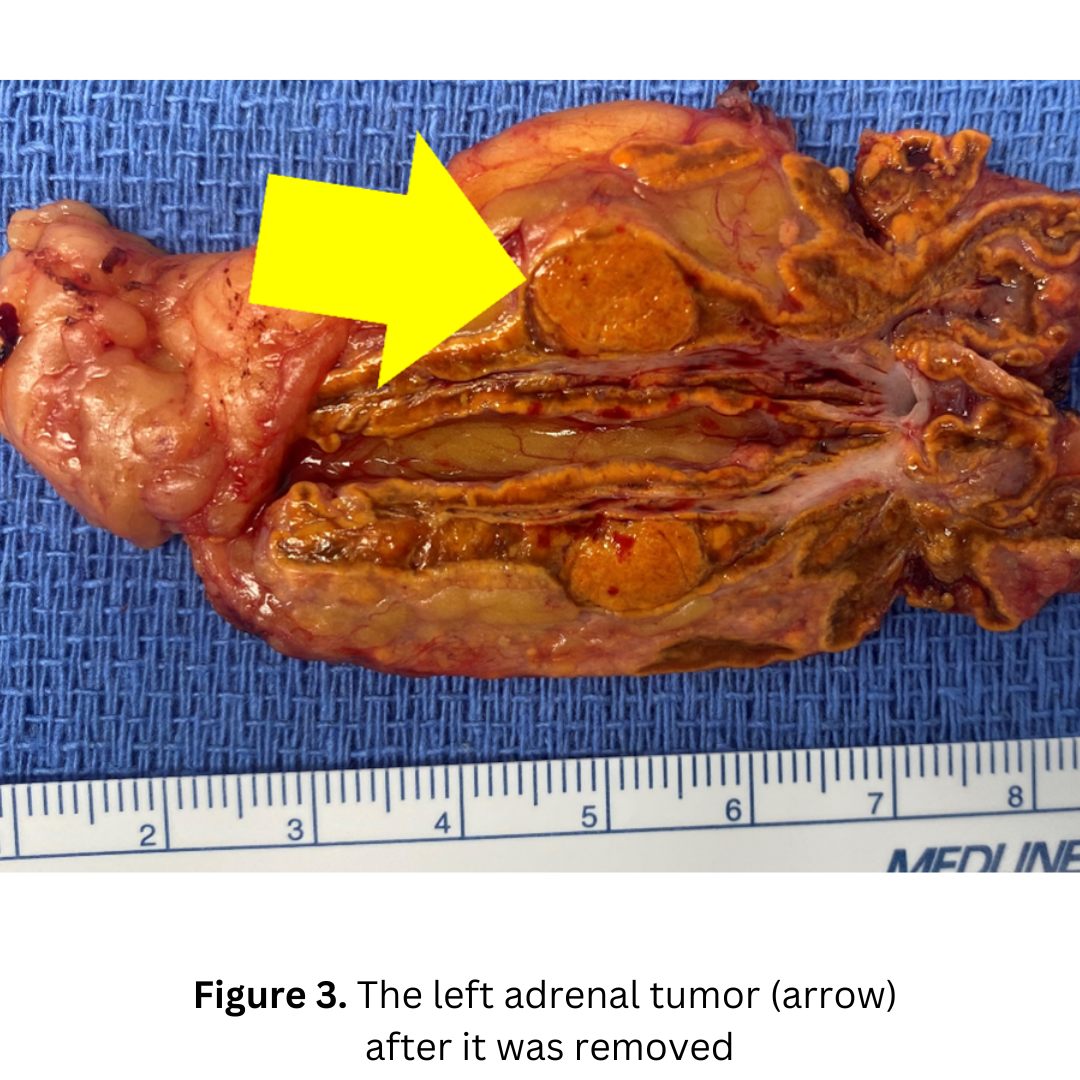
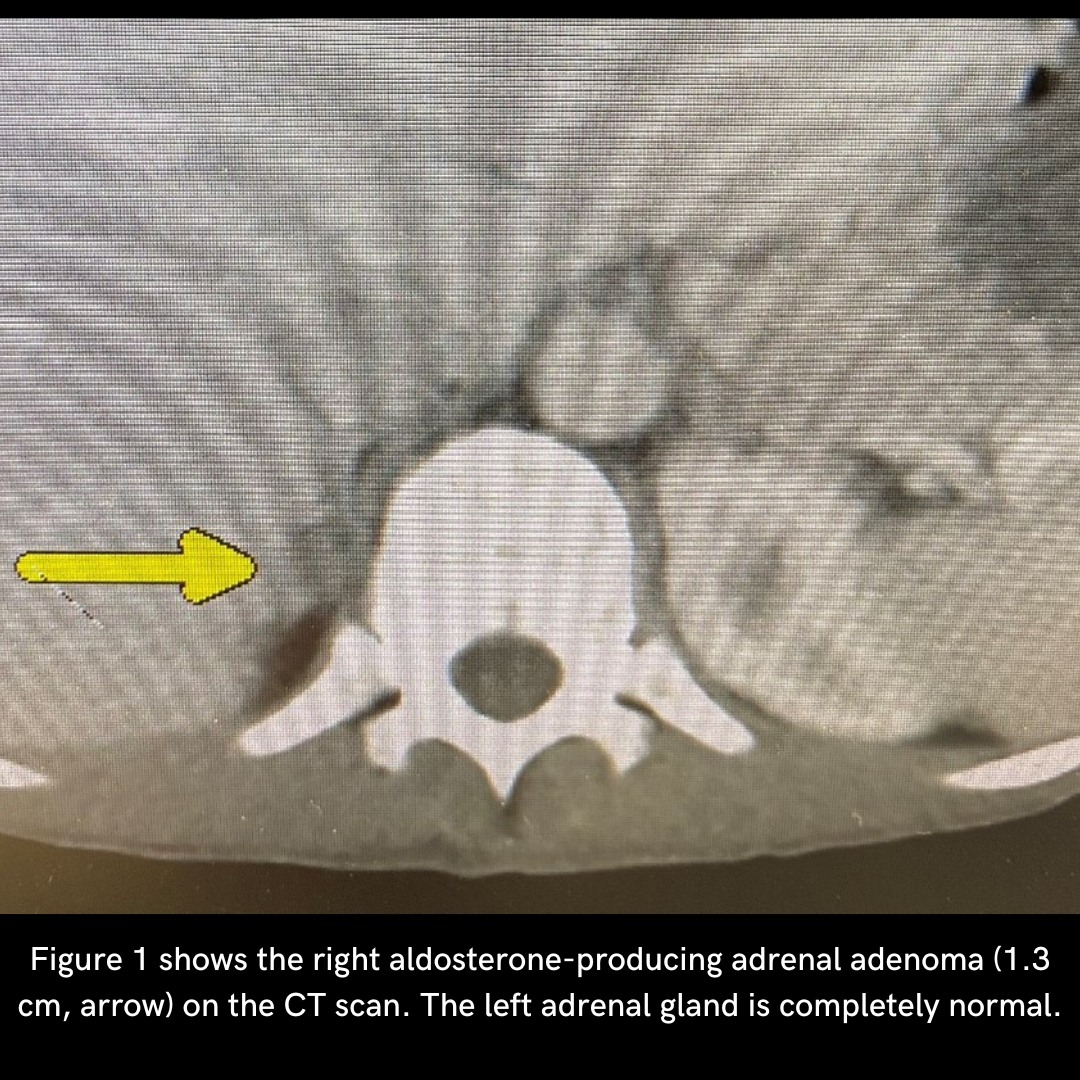
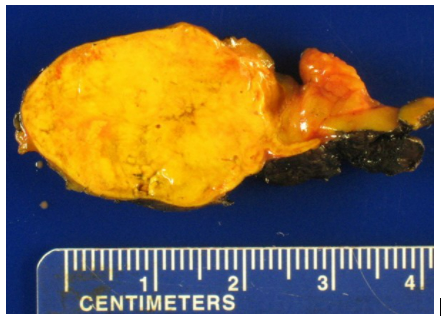
The second photo shows the left aldosterone-producing adrenal adenoma (1.2 cm, arrow) on the CT scan. The right adrenal gland is completely normal.
Our patient had a mini back scope adrenalectomy (MBSA) that took just 23 minutes. After a healthy breakfast on our hospital terrace in the morning Florida sunshine, he was on his way to explore some of the Tampa Bay sights prior to flying home.
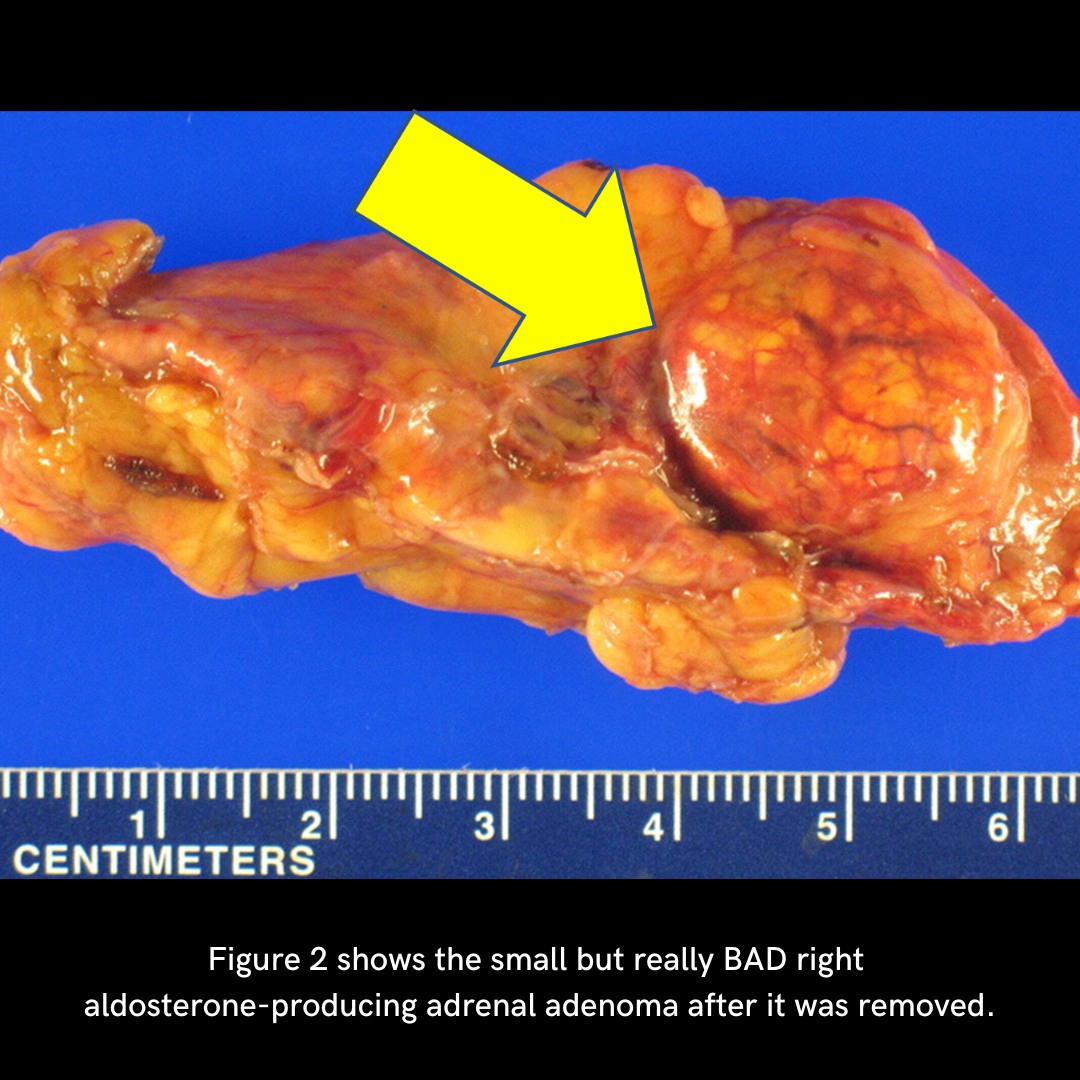
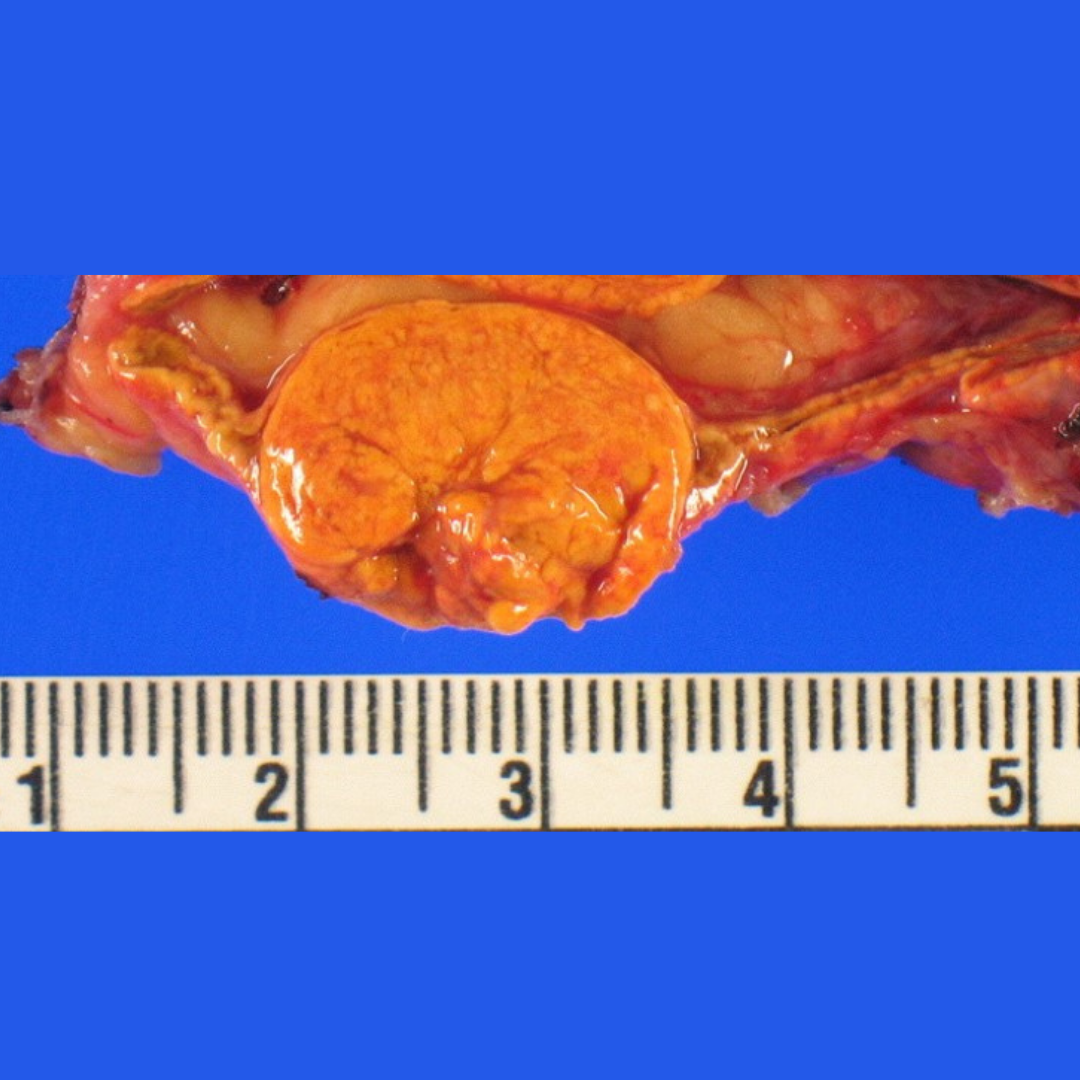
The last photo shows the small but very bad left aldosterone-producing adrenal adenoma after it was removed.
Interesting case of the week: Subclinical Cushing’s syndrome due to tumors in both adrenal glands
Cushing’s syndrome, or too much cortisol, is probably the one disease that confuses the most doctors, nurses, and patients. But when it comes to adrenal Cushing’s syndrome, it is actually quite straightforward. Adrenal Cushing’s syndrome means too much cortisol that originates from the adrenal gland. Sometimes doctors do it all correctly and diagnose adrenal Cushing’s syndrome, but then when they see scans showing tumors on both adrenal glands they get confused.
Many surgeons would only remove one adrenal gland. This does provide some benefit for the patient, but it is not nearly as good as addressing both adrenal tumors by partial adrenalectomy. The Cushing’s syndrome is only completely cured if both tumors are removed.
Today's patient is a 71-year-old woman who struggled with adrenal Cushing’s syndrome for years. She was experiencing heartburn, excessive hair loss, high blood pressure and diabetes.
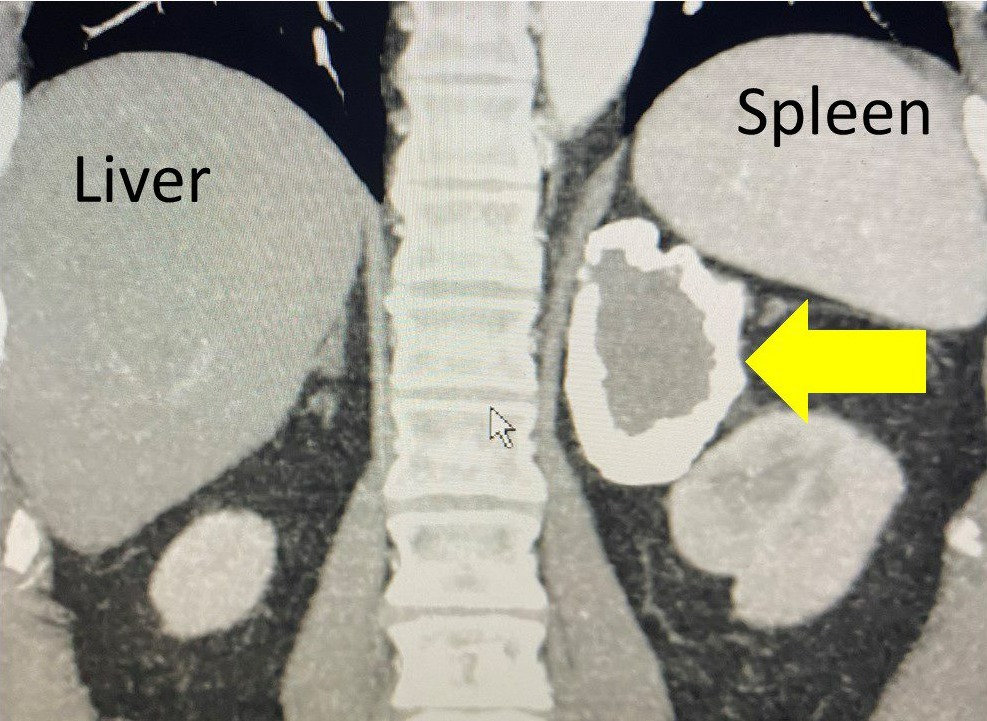
She had a Low Dose Dexamethasone Suppression Test that was abnormal (meaning Cortisol in the morning >1. Her ACTH (pituitary hormone) was completely suppressed and her 24 hour urine free (UFC) cortisol was on the high side. She then underwent a CT scan that showed a large mass on the left adrenal gland measuring 6.8 cm, but she also has a 1.4 cm mass on the right adrenal.
Figure 1: The CT scan demonstrates bilateral adrenal tumors, the left larger (6.8 cm) than the right.
For this patient, the best option was to deal with the large left adrenal mass first. She underwent a 21-minute Mini Back Scope Adrenalectomy (MBSA) on the left side.
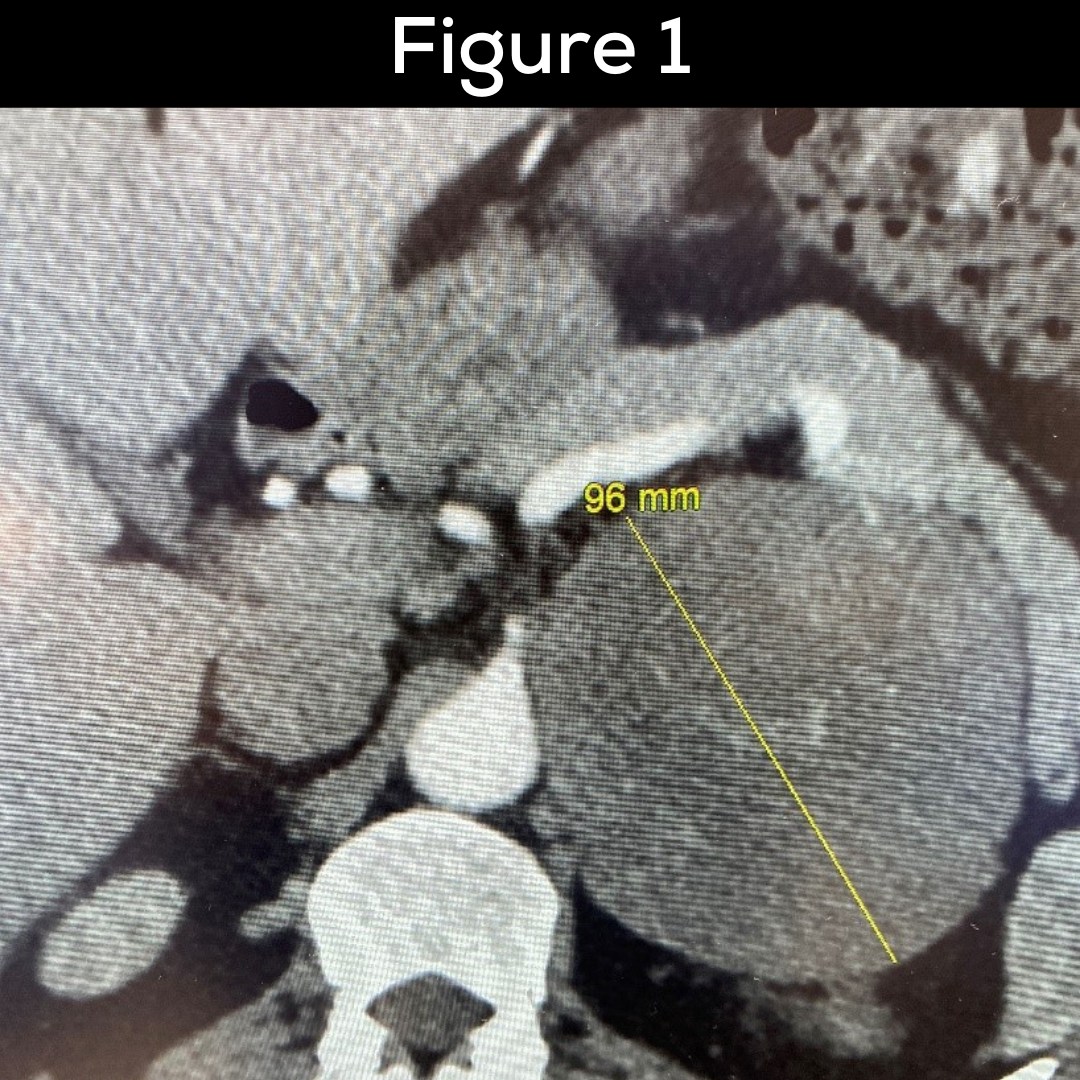
Figure 2. The large left cortisol-producing adrenal tumor.
In six weeks, we will go back and remove the tumor on the right adrenal gland. Both sides will have a partial adrenalectomy (cortex sparing) approach, and spacing the operation out over six weeks allows her not to have to be dependent on any steroid hormones. This is great news for our patient!
Interesting case of the week:
As we are wrapping up adrenal disease awareness month, we are meeting Dawn from Kansas City, MO. Dawn has suffered from Cushing’s Disease for close to two decades and has undergone two failed pituitary operations, brain radiation to the pituitary and medical treatment. She came to the Carling Adrenal Center for a bilateral adrenalectomy because of “failed” Cushing’s Disease.
In this video, Dr. Carling chats with Dawn about her experience with Cushing's Disease, treatment, surgery and more.
At the end of the video, you'll see a photo of Dawn’s adrenal glands after removal. The operation lasted about 15 minutes on each side, meaning about 30 minutes for both adrenal glands.
Read more about the
best treatment for Cushing's disease.
The Mini-Back Scope Operation (MBSA) is the best adrenal operation for “failed” ACTH-dependent Cushing’s disease. Do not go through the belly to get to the adrenal glands!

Interesting case of the week: Old pheochromocytoma tumor in patient from Hongkong
Our patient is a 56-year-old man with a known right adrenal tumor diagnosed 10 years ago. Nothing was done about it at the time. He did not have the required follow up. In retrospect, he should have had adrenal surgery 10 years ago.
He lives in Hongkong, and was now suffering from heart palpitations, pre-diabetes, hyperlipidemia, tremors, excessive sweating, panic attack symptoms, and dizziness. His catecholamines, normetanephrines and metanephrines were all very high (more than 10x normal).
He was a textbook case of pheochromocytoma.
Learn more about the symptoms of pheochromocytoma here.
He contacted us at the Carling Adrenal Center, and within days was on a flight from Hongkong to Tampa. His endocrinologist locally had already started him on a medication called alpha-blocker, so he was immediately ready for surgery. He had seen the most experienced adrenal surgeon in Hongkong. Unfortunately, the surgeon only performed the operation through the belly.
The patient had a mini back scope adrenalectomy (MBSA) which took 26 minutes. Can you imagine traveling across the planet for a 26-minute operation? Well trust me... It’s a lot better than traveling 20 minutes to the hospital down the street to have an eight-hour long operation involving a robot and with complications (or worse).
The patient had the best operation for pheochromocytoma.
Fortunately, the patient made the trip into a little bit of a mini vacation and will enjoy the beautiful spring in Florida and a trip to visit his family in the Northeast prior to heading back to Hongkong. We were all honored to take care of him and get him cured of his pheochromocytoma!
Interesting case of the week: 25-year history of small aldosterone-producing tumor causing stroke and kidney disease
Every week I see multiple patients who clearly have had their adrenal tumor disease for years and decades. The disease has either not been diagnosed at all or just managed with ineffective medications.
The patient is a very sweet 82-year-old man who had been suffering with Conn’s syndrome or primary hyperaldosteronism for at least 25 years. When he was younger, he developed high blood pressure which he'd been managing with five different blood pressure medications and extra potassium for decades.
We were able to track down a CT scan he had almost 20 years ago and, no surprise, the left adrenal tumor was present back then. His lab test clearly showed his aldosterone levels to be very high and his renin levels to be low. It's obvious what was going on... This patient has had primary hyperaldosteronism due to a left aldosterone-producing tumor.
He was treated with one pill after another until a smart endocrinologist figured out what was going on. Unfortunately, he had already developed many complications from primary hyperaldosteronism. He had a stroke and has stage 3 chronic kidney disease (CKD). If he would've had surgery 20 years ago, this could easily have been prevented.
Read about complications of primary hyperaldosteronism and Conn’s syndrome here.
The adrenal adenoma was removed by a 24-minute Mini Back Scope Adrenalectomy (MBSA).
The photo shows the pathology of the 11 mm aldosterone producing adrenal adenoma.
He will benefit greatly from having his aldosterone levels normalized.
Interesting case of the week: Cushing’s Disease – Adrenal Gland Removal after “Failed” Pituitary Surgery
April 8 is Cushing's Disease Awareness Day!
In recognition, we are following up with a young 22-year-old UCLA student who underwent a bilateral adrenalectomy (BLA) because of “failed” Cushing’s Disease about 6 months ago.
You can watch her initial video here.
Overall, she has done tremendously well since surgery. Watch the full Q&A to hear her discuss her long journey with Cushing's Disease, her surgery experience and her new and improved life.
The first-line treatment for Cushing’s disease is pituitary surgery to remove the tumor. When pituitary surgery works (70%), it is great! However, about 1/3 will never be cured in the first place or the tumor grows back (recurrence). This is “failed” Cushing’s Disease. Don’t despair! There are other treatment options.
In these patients, removing all cortisol-producing cells (total bilateral adrenalectomy) is often the best option. The goal is to remove all cells of the adrenal glands, which overproduce the toxic levels of cortisol.
The Mini-Back Scope Operation (MBSA) is the best adrenal operation for “failed” ACTH-dependent Cushing’s disease. Do not go through the belly to get to the adrenal glands!

Interesting case of the week: An Update from a lovely patient!
Today's interesting case is an update from one of our favorite recent patients! Sara, a pregnant adrenal pheochromocytoma patient, underwent a mini back scope adrenalectomy (MBSA) with Dr. Carling a few months ago.
She then sat down with us for a Q&A about her diagnosis, how she chose the Carling Adrenal Center, her surgery experience, her recovery and more.
You can watch the full Q&A here.
Our entire team was so excited for Sara and requested an update from her when the baby was born, and she was kind enough to send us this halfway update!
"Since July/August is still a ways off, I thought a halfway there pregnancy update might be appreciated! We had our 20 week gross anatomy scan last Friday and baby appears healthy and is growing and developing normally. He or she even gave us a thumbs up (see ultrasound)! All my providers continue to be so impressed with how things turned out and Dr. Carling’s minimally invasive strategy to remove my adrenal tumor. Those who weren’t already aware of him have said they are sticking his name in their back pocket for any future adrenal patients needing surgery they may encounter."
We can't wait to hear from Sara later this summer and see photos of her beautiful baby!
The Carling Adrenal Center is a worldwide destination for the surgical treatment of adrenal tumors. Founded by Dr. Tobias Carling MD, PhD, the center performs more adrenal surgery than any other hospital in the world.
Interesting case of the week: Subclinical Cushing’s syndrome patient traveled all the way from Australia!
Interesting case of the week: Subclinical Cushing’s syndrome patient traveled all the way from Australia!
There are a lot of healthcare providers that do not know enough about Cushing’s syndrome. This is not only true in America, but it is true in Europe, Australia, and all throughout the world. Many doctors think it is a very rare disease and that adrenal tumors do not need to be taken seriously.
This week's patient came to us all the way from Australia. She is the first patient with an adrenal tumor from Australia to be operated on at the brand the Hospital for Endocrine Surgery, which opened in Tampa in January 2022.
She had a long journey. She flew from her hometown in Queensland to Sydney, then from Sydney to Dallas, and finally to Tampa.
When you have subclinical Cushing’s syndrome, it is due to a tumor of the adrenal gland that is producing too much cortisol. Too much cortisol can cause a lot of symptoms. This patient was experiencing heartburn, heart palpitations, leg and arm cramps, muscle weakness, decreased sex drive, difficulty concentrating, difficulty with memory, facial rounding and plethora, supraclavicular and dorsocervical fat pads (fat deposits on the back; 'buffalo hump'), easy bruising, poor wound healing, stretch marks, anxiety, hirsutism (excessive facial hair), low blood potassium (hypokalemia), weight gain with central obesity (meaning unusual fat deposition around your abdomen), excessive sweating, panic attack symptoms (fear, anxiety).
Read about symptoms of Cushing’s syndrome here.
Her doctor had tried her on a medication called for fluconazole. Fluconazole is really an anti-fungal medication. It works very well for fungi and other yeast infections. However, it has a side effect of affecting the cortisol production from the adrenal gland. Like any other medications for Cushing’s syndrome, the medication does not help the root cause. Medications do not remove the tumor. They just temporarily lowers the cortisol in your body. Medications do not work and made our patient ill.
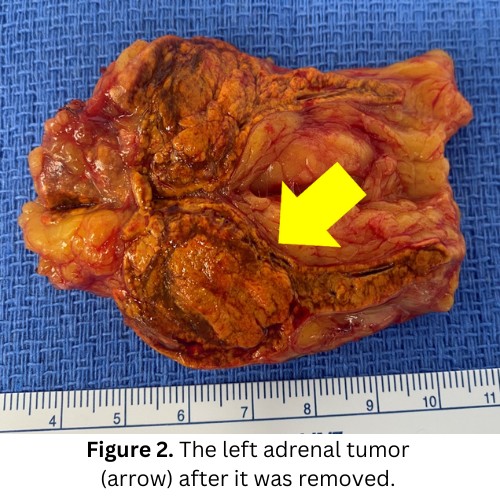
Figure 1: Her CT scan showing the left adrenal mass
The patient had a mini back scope adrenalectomy which took 22 minutes. Can you imagine traveling for two days to have a 22-minute operation? Well, trust me... It’s a lot better than traveling 20 minutes to the hospital down the street to have an eight-hour long operation with complications (or worse).
Figure 2: The left adrenal tumor
Fortunately, the patient made the trip into a mini vacation and will enjoy Florida's beautiful springtime!
Interesting case of the week: Removing an adrenal tumor and parathyroid tumor at the same visit!
Today's patient is a 61-year-old lady who is local from Florida. She presented with signs of symptoms of bone pain, fatigue, insomnia, difficulty sleeping and problems with concentration. She had had a CT scan that indicated a 2.5 cm right adrenal mass.
She had a proper work up and everything was negative except that there was an indication that she had slight cortisol overproduction. Her ACTH level was low, and she failed her low-dose dexamethasone suppression test. This indicated Subclinical Cushing’s syndrome.
Learn more about Subclinical Cushing’s syndrome.
Interestingly, the patient also had by chemically unequivocal primary hyperparathyroidism. Her calcium had been ranging between 10.7-10.9 mg/dl and the parathyroid hormone (PTH) was non-suppressed at 58 to 59 ng/l. Her vitamin D levels, and creatinine were all normal. This proves that the patient not only have subclinical Cushing’s syndrome from a right adrenal mass but also a parathyroid tumor causing primary hyperparathyroidism.
You may not know, but parathyroid tumors were Dr. Carling‘s first love when it came to endocrine surgery. In fact, he defended his PhD dissertation in 1997 with a thesis entitled “Vitamin D receptor and estrogen receptor gene polymorphisms in primary hyperparathyroidism”. As a 23-year-old, he published his first paper on parathyroid tumors and primary hyperparathyroidism in Nature Medicine (one of the world’s most prestigious scientific journals). In addition to being the world’s #1 top adrenal surgeon, Dr. Carling is not only one of the most prominent scientists when it comes to primary hyperparathyroidism and parathyroid tumors, but has also performed thousands of parathyroid operations. Nowadays, he spends two full days doing up to 6 to 8 adrenal operations each day for two days, but he loves parathyroid surgery so much that he saves one full day for parathyroid surgery still. He and his team do up to 30 parathyroid operations in that single day! This is >95% of American hospitals perform in a year.
So, what could be better? Getting both your adrenal tumor and parathyroid tumor fixed at the same time!
Figure 1 shows the right adrenal tumor measuring about 2.5 cm.
The tumor was easily removed using the mini back scope adrenalectomy (MBSA). The operation was very straight-forward and took 13 minutes.
Read more about the mini back scope adrenalectomy (MBSA) here.
The patient spent one night in the hospital to make sure that her heart rate and blood pressure as well as cortisol was fine the next morning.
She then went down for her parathyroid surgery.
Figure 2 shows a very typical right upper parathyroid adenoma of the ultrasound that Dr. Carling performed before the operation.
At the Norman Parathyroid Center, we perform all operations with two surgeons. We have a very unique and (in my mind) excellent philosophy. We believe in the team approach and putting our ego aside, we make sure that at least two world-class surgeons perform each surgery.
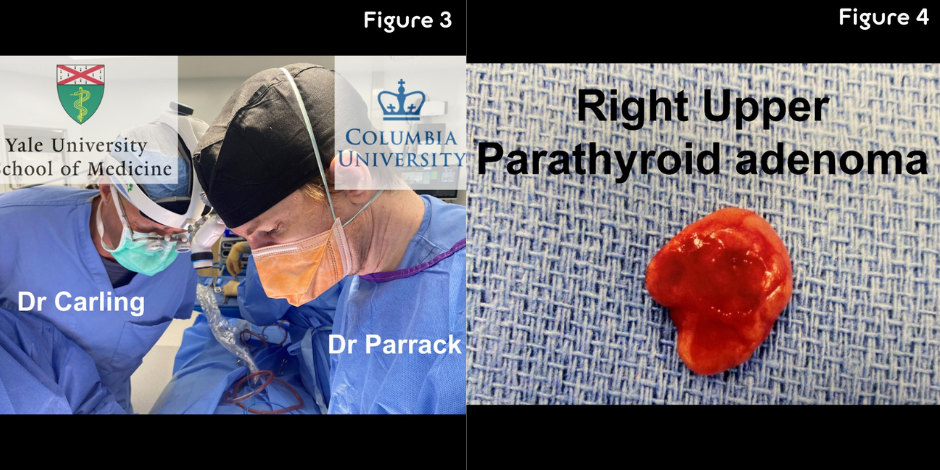
Figure 3 shows Dr. Carling and Dr. Parrack, working together on this patient making sure we are not the only removing the parathyroid adenoma, but also identifying and evaluating the other three parathyroid glands, which in this case were all normal. This mini-parathyroid operation took 15 minutes. Usually, Yale and Columbia are rivals in the Ivy leagues but here we work together for the best of the patient!
Figure 4 shows the parathyroid tumor (adenoma) which is approximately 30 times normal after was removed. The patient’s parathyroid hormone (PTH) level in the recovery room was 14, which is exactly where Dr. Carling wants it to be. This proves that the patient is now cured from her primary hyperparathyroidism as well as her subclinical Cushing syndrome.
It is definitely worth it to travel from around the world to Tampa to have the best possible surgery by the Carling Adrenal Center and Norman Parathyroid Center.
Interesting case of the week: Another young lady from California with Conn's syndrome
For some reason, recently we have had several young patients from California with adrenal tumors. Today we have a 33-year-old, otherwise super healthy, young lady. She is a young mom and has a six-year-old who was delivered by C-section in 2016. She had no problems with high blood pressure during the pregnancy but the last 2-3 years she started to have high blood pressure in addition to many other symptoms. She had problems with heart palpitations, leg and arm cramps, muscle weakness, problems with concentration and memory, irritability, reduced sex drive, low potassium, pallor, excessive sweating, and problems with dizziness. These are all common symptoms from primary hyperaldosteronism and Conn’s syndrome.
Read about symptoms of primary hyperaldosteronism and Conn’s syndrome here.
Fortunately, she saw a smart cardiologist who thought it made no sense that an otherwise super healthy and slender 33-year-old young mom should have those symptoms along with very high blood pressure. They accurately measured the aldosterone level, which was high, and the renin level, which was very low. This proved that she had primary hyperaldosteronism or Conn’s syndrome. They also obtained a CT scan that showed a typical right adrenal mass measuring about 1.7 cm. Importantly, the left side was completely normal.
Figure 1 shows the aldosterone-producing adrenal adenoma (1.7 cm, arrow) on the CT scan.
This is as textbook “slam dunk” Conn’s syndrome or primary hyperaldosteronism comes. This patient does not need adrenal vein sampling (AVS) or any other test.
Fortunately, she probably only had this tumor for a few years and was spared kidney failure, strokes, heart attacks and heart arrhythmia.
Read about long-term complications of untreated (or just BP medications) Conn’s syndrome here: The aldosterone-producing adrenal adenoma was successfully removed through a 14-minute Mini Back Scope Adrenalectomy (MBSA).
Read more about the mini back scope adrenalectomy (MBSA) here.
This patient is now completely cured of her primary hyperaldosteronism and Conn’s syndrome and is doing very well! She is ready to get on with her life and do all the fun things she used to do.
From our lovely patient:
"I will forever be grateful for Dr. Carling. Your enthusiasm, knowledge, and dedication regarding adrenal illness is unmatched. I am feeling like my old self again! Blood pressure has returned to normal, headaches have ceased, and fatigue is now a thing of the past. I have attached a picture that I absolutely love. Please feel free to share it however you please. I am very proud of it, as you should be too! Stay well and keep changing lives for the better."
Remember, if you are a young patient (meaning less than 50 years old) and you do not have any significant risk factors (smoking, diabetes, obesity, etc.), there is no reason you should have high blood pressure. Do not give up! You are your own best advocate.
Interesting case of the week: Pheochromocytoma of the neck - you are kidding!
Can you have a pheochromocytoma of the neck? Well, yes and no.
Paragangliomas, or carotid body tumors, are neuroendocrine tumors that arise close to the main artery of your neck, called the common carotid artery. They are called paragangliomas or carotid body tumors. However, they arise from the same cell types as pheochromocytomas from the medulla of the adrenal gland so in essence they are pheochromocytomas of the neck. So yes, you sort of can have a pheochromocytoma of the neck!
Read more about pheochromocytomas here.
The patient is a 69-year-old woman from Idaho. She had known paraganglioma of her right carotid body for many years. It had plagued her significantly and she had a lot of symptoms with tremors, excessive sweating, panic attacks with anxiety and dizziness especially with standing. Those are all very typical symptoms of paragangliomas (carotid body tumors) of the neck.
Her doctors checked her hormone levels including adrenaline-type hormone (metanephrines and normetanephrines) and they were only mildly elevated. However, this is quite typical in neck paragangliomas and carotid body tumors. Patient can still have a lot of symptoms, though!
She traveled around the Mountain West and the West Coast of United States and every surgeon she saw at the at the major university hospitals were too afraid to operate on her, so she contacted us.
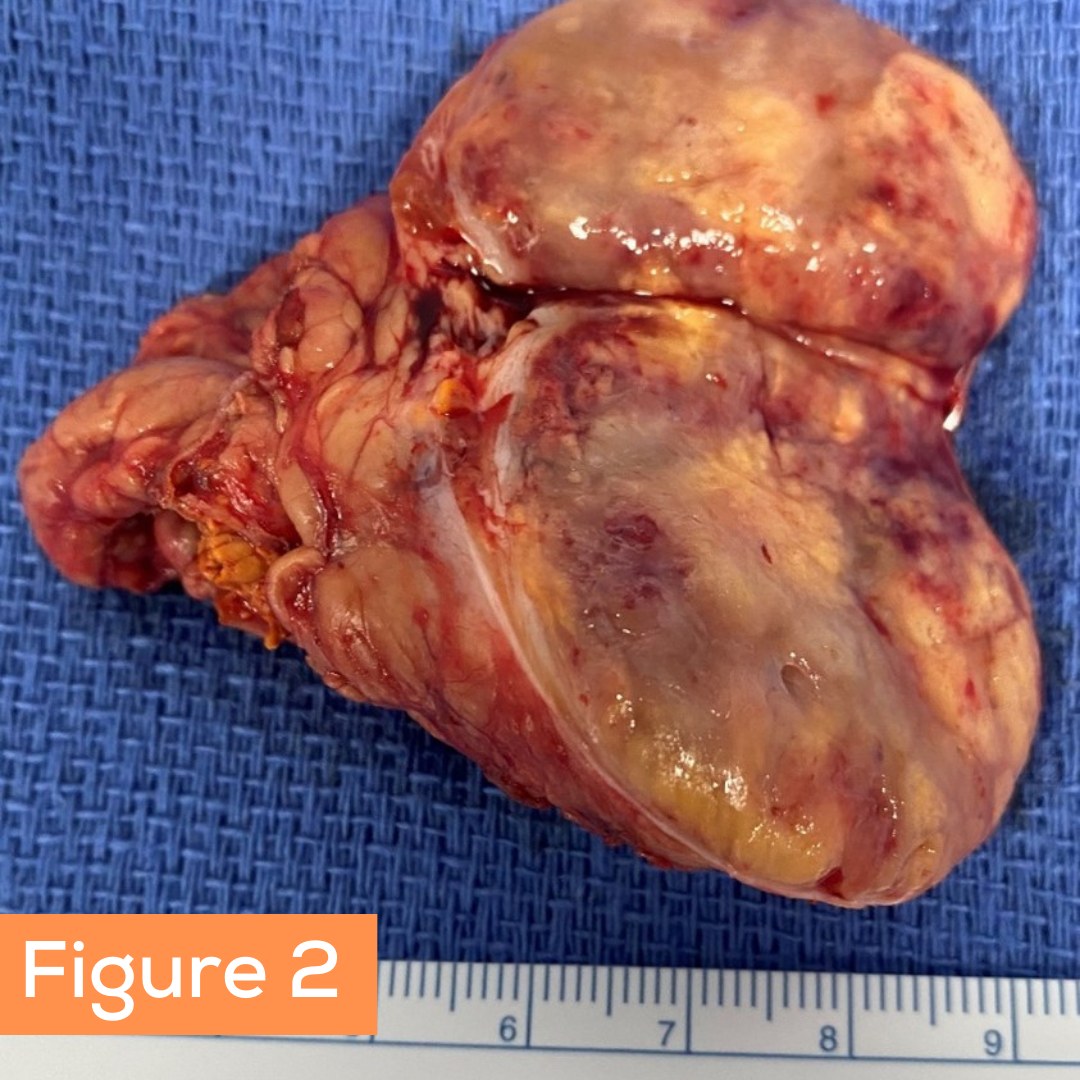
What is better than having the best pheochromocytoma and paragangliomas surgeon taking care of you? How about two of the world's best surgeons working on you.
Dr. Carling (Carling Adrenal Center) and Dr. Clayman (Clayman Thyroid Center, and an expert in advanced head and neck cancer) decided to work together on this case. They literally operate next to each other every day. This is an example of the beauty of the Hospital for Endocrine Surgery. You have the top 11 endocrine surgeons in the world when it comes to adrenal, parathyroid and thyroid disease all working in a cohesive manner literally side by side.
Dr. Carling consulted with the patient over the phone and reviewed the images together with Dr. Clayman and the patient flew down to Tampa for her surgery.
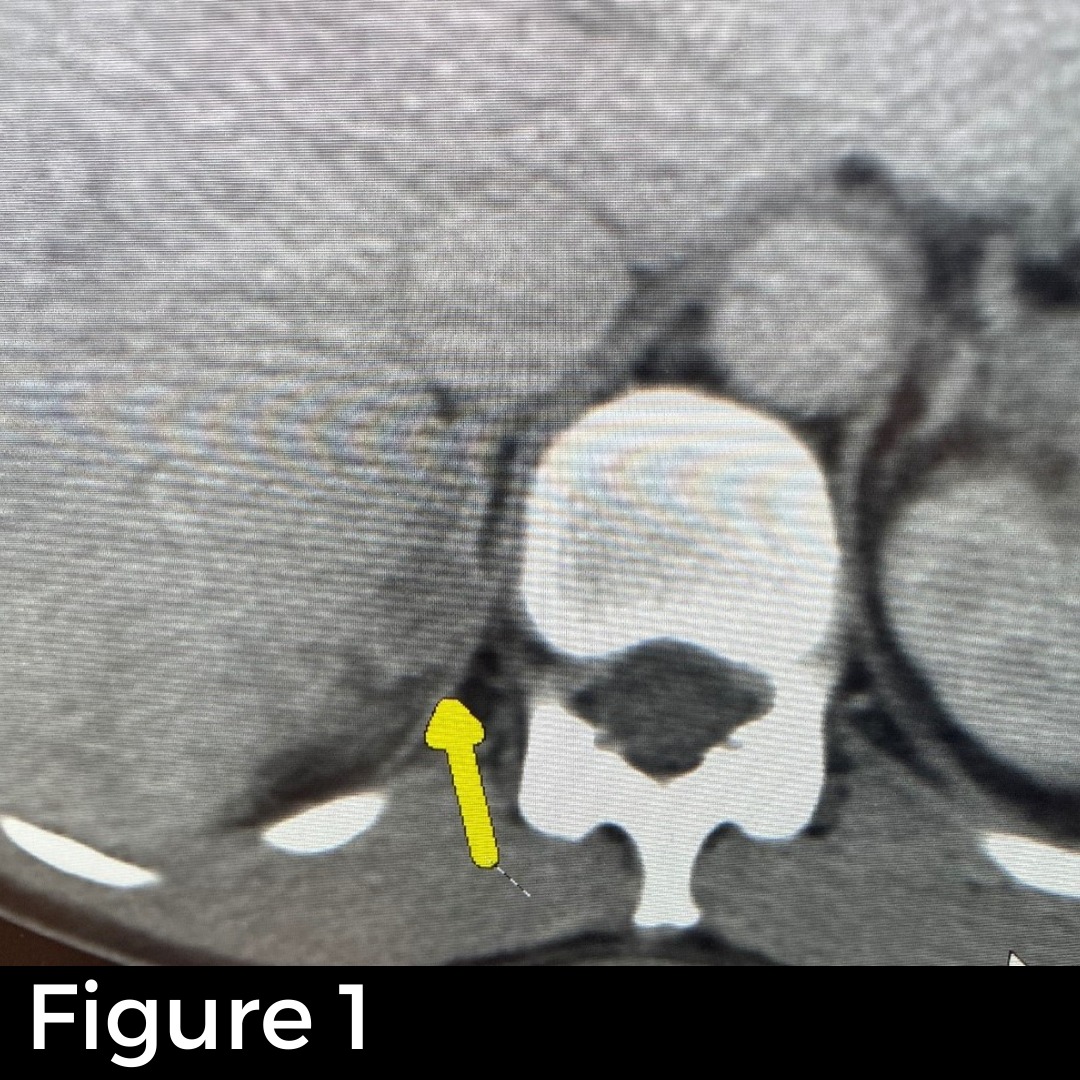
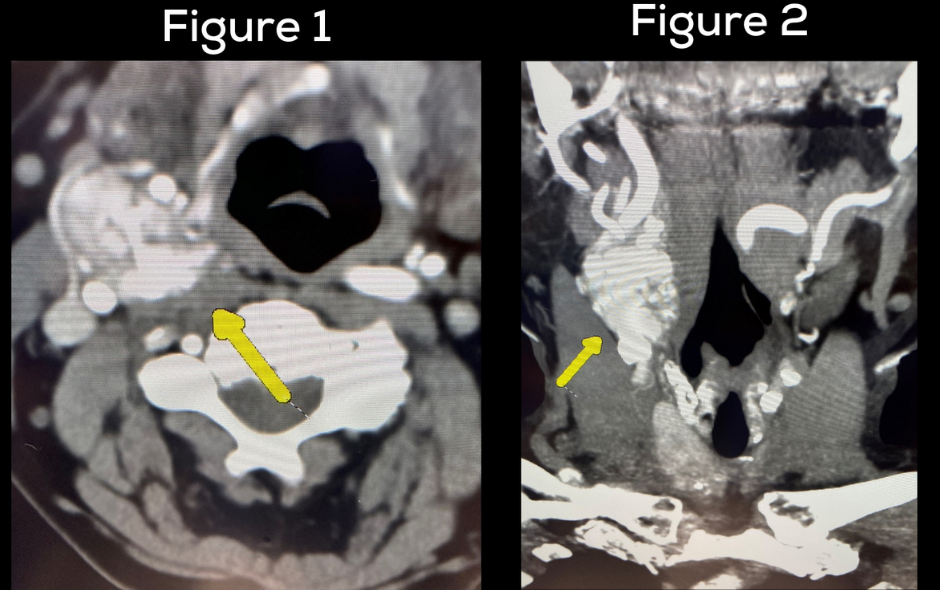
Figures 1 and 2: You can see her right carotid body tumor, paraganglioma. A yellow arrow indicates the tumor. As you can see the tumor is very vascular and all the major vessels including the internal jugular vein the common carotid artery, the external carotid artery (ECA) and, the internal carotid artery (ICA) are all intimately involved with the tumor. The tumor is literally splitting the ICA and ECA apart
Figure 3 shows Dr. Carling and Dr. Clayman working very meticulously but efficiently removing the tumor. In the end, the patient (who had been declined surgery at many famous medical institutions) had the tumor removed by Dr. Carling and Dr. Clayman in under an hour, very safely.
Figure 4 shows the operative field after that the dissection. It shows the internal jugular vein (IJV) the common carotid artery (CCA) as well as the internal carotid artery. The nerve number X (vagus nerve) and the nerve number XII (hypoglossal nerve). The vagus nerve controls your voice, and the hypoglossal nerve controls the function of the tongue. All important vessels and nerves were completely preserved, and the patient had perfect function afterwards.
Interesting case of the week: Large adrenal cancer with too much cortisol and estrogen
The patient is a 55-year-old man from Miami. Over the previous months he had noticed gynecomastia (breast tissue developing in a man), tiredness, and decreased libido (sex drive). He had actually seen a surgeon to have his breast tissue removed (never performed, fortunately), but via a circuitous route was referred to an endocrinologist.
This doctor understood what was going on and ordered laboratory test and an MRI scan of his abdomen. The laboratory test showed very high cortisol levels (Cushing’s syndrome, causing his fatigue) and high estrogen levels (leading to feminization causing breast development and decreased sex drive). The MRI demonstrated a huge left adrenal mass.
Read more about symptoms of adrenal cancer here.
The patient had seen a number of surgeons and been recommended everything from biopsies (don’t get me started #1), to radiation and chemotherapy (don’t get me started #2). What this patient needed was an operation.
Read why adrenal biopsy are a huge mistake in almost all patients here.
Chemotherapy should never be used unless surgery is no longer an option.
Figure 1 shows the huge mass (> 10 cm) of the left adrenal gland on the CT scan.
Figure 2 shows the breast development in a man (gynecomastia) on the CT scan (yellow arrows).
This case illustrates the less than 3 % of patients where the mini back scope adrenalectomy (MBSA) is not the appropriate operation. The best operation in this case is the laparoscopic transabdominal hand-port assisted adrenalectomy, which is the operation he had. Although the tumor was very close to some major structures and vessels (stomach, pancreas, colon, left kidney, spleen, splenic artery and vein, and renal artery and vein), all those structures were preserved and there was zero blood loss.
We have already set up a team of doctors who will keep a very close eye on him for many years to come. His gynecomastia and Cushing’s syndrome will be cured and slowly disappear. His libido will return.
Become Dr. Carling's patient at the Hospital for Endocrine Surgery here.
Interesting case of the week: 21 years old and dealing with a Pheochromocytoma!
Ahhh…remember back when you were 21 years old… You were strong, had endless energy, and the whole life ahead of you. You had probably just started working your first job or you were studying at college or university.
The last thing on your mind was worrying about being sick, especially by an adrenal tumor spewing out toxic levels of dangerous hormones.
Well, meet one of my recent patients. He is 21-years-old. For some time before coming to the Carling Adrenal Center he had experienced heart palpitations (strong heart beats), excessive sweating and episodes of elevated blood pressure. Fortunately, he had a smart cardiologist who took his symptoms seriously and ordered labs. His catecholamines and metanephrines (adrenaline-type hormones) were more than 10 times normal. An MRI demonstrated a 4.1 cm left adrenal mass. The diagnosis of left adrenal pheochromocytoma was established.
Fortunately, our 21-year-old was one of our local patients and lived only about 3 hours’ drive away (we regard anyone living in Florida as “local” patients). He was started on an alpha blocker called Phenoxybenzamine until he was ready for surgery. His mom was a bit nervous because she was told (by health care professionals) that the pheochromocytoma could burst. Pheochromocytoma do not burst while on alpha blockers. In fact, we have patients with pheochromocytomas flying in from all over the United States and the world for surgery, and they all do just fine. However, if the catecholamines and metanephrines (adrenaline-type hormones) are >5 times elevated we like them to be on an alpha blocker medication prior to surgery and when they travel to Tampa.
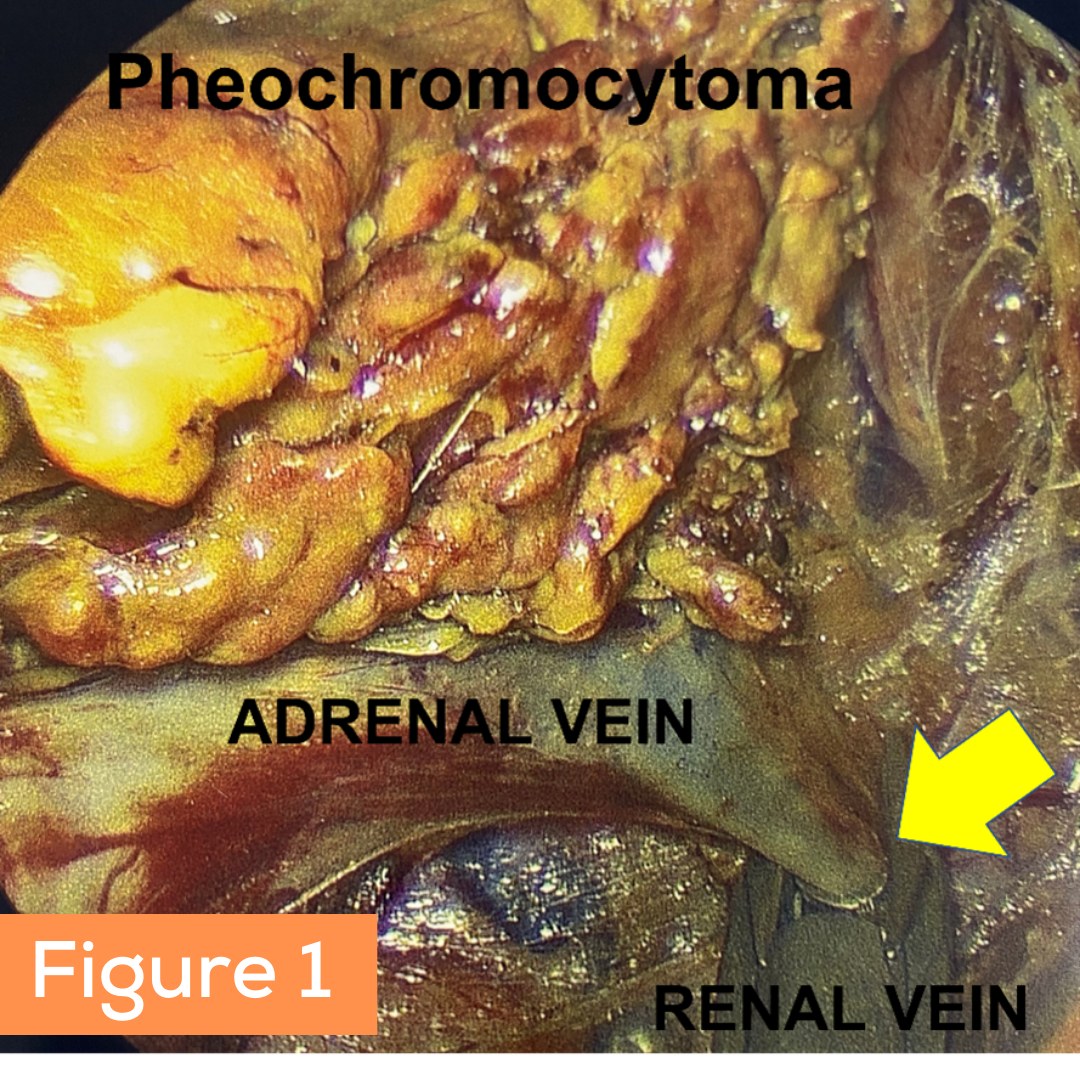
Figure 1: This photo was taken with an endoscope which is the type of camera Dr. Carling uses in the operating room. The left adrenal vein draining the pheochromocytoma can be seen and Dr. Carling has placed a clip (yellow arrow) so it can be divided off the left renal vein. As you can imagine it requires superb skill to do this operation perfectly.
Figure 2: The bad pheochromocytoma tumor can be seen here.
He had an 18-minute mini back scope adrenalectomy (MBSA). He is now cured. This is a done deal, and he can get back to doing all the fun things a 21-year-old young man should do!
Become Dr. Carling's patient at the Hospital for Endocrine Surgery here.
Interesting case of the week: Calcified Adrenal Mass with Dr. Tobias Carling
The patient is a 57-year-old woman who had a known left adrenal mass, which likely was related to a previous episode of bleeding (hemorrhage). Bleeding in a normal adrenal gland or a pre-existing tumor can be problematic. As the area heals, it sometimes forms a peripherally calcified mass, meaning, there is calcification formed at the outer layer of the adrenal mass.
The mass occasionally bothered her with pain in the area. The patient’s laboratory investigation was normal, except for low cortisol levels. However, she had chronically been maintained on hydrocortisone for cervical disc disease, which explained this.
The tricky thing with adrenal tumors containing calcifications is that we can see this in both benign and cancerous cases. Adrenal cortical adenomas, adrenal carcinomas, previous adrenal hemorrhage, adrenal metastases, pheochromocytomas, and some infectious processes of the adrenal all can manifest as a calcified mass
She underwent a CT scan which you can view in the photos shown here. The yellow arrow indicates the large left adrenal mass.
Read more about imaging and best X-ray studies of adrenal tumors here.
Reviewing the CT scan made me quite confident that this was a not cancerous. However, when these masses are symptomatic (as in our patient’s case) they need to be removed by surgery.
The patient was an excellent candidate for the mini back scope adrenalectomy (MBSA), and did tremendously well after the operation.
Read more about the mini back scope adrenalectomy (MBSA) here.
Next, she will work with her endocrinologist to wean off her hydrocortisone. Unfortunately, she was placed on steroid for her cervical disc disease, and now her right adrenal gland (the one remaining) is iatrogenically suppressed by long term steroid use. Over time it will wake up, but it may take several months. Don’t stay on steroids longer than you absolutely have to!
Become Dr. Carling's patient at the Hospital for Endocrine Surgery here.

Interesting case of the week: Cystic Adrenal Mass with Dr. Tobias Carling
A mass that is cystic means that it contains fluid. Cystic adrenal masses are not uncommon. They include benign cysts like endothelial and epithelial adrenal cysts, as well as pseudocysts. However, actual tumors such as adrenal cortical adenomas and cancers can contain cysts. Pheochromocytomas famously can be cystic, as well.
This week’s patient is a 59-year-old woman who noticed some pain in her left abdomen. She also had some blood in her urine.
She underwent a CT scan, which you can view in the photos here. The yellow arrow indicates a large 7 cm cystic adrenal mass.
Reviewing the CT scan made me quite confident that this was a typical simple cyst, and she had no risk of it being a tumor. However, even simple cysts can sometimes cause problems. The most common symptom is abdominal pain or other GI tract symptoms. When these cystic masses are symptomatic (as in this case) they need to be removed by surgery.
The patient was an excellent candidate for the mini back scope adrenalectomy (MBSA). The patient had this mass removed in a 19-minute, straightforward operation. She quickly returned to normal activities and is doing well. Once the adrenal cyst is completely removed, it will never return.
Read more about the mini back scope adrenalectomy (MBSA) here.
The Carling Adrenal Center is a worldwide destination for the surgical treatment of adrenal tumors. Founded by Dr. Tobias Carling MD, PhD, the center performs more adrenal surgery than any other hospital in the world. The Center is located within the famous Hospital for Endocrine Surgery in Tampa, Florida.
Become Dr. Carling's patient at the Hospital for Endocrine Surgery here.

Interesting case of the week: Our first adrenal tumor pateint at the brand-new Hospital for Endocrine Surgery!
The Hospital for Endocrine Surgery is the only hospital of its kind in the entire world. It is a full-fledged hospital with an Emergency Department (ER) and in-hospital beds (not a “surgery center”). The hospital is dedicated solely to patients with adrenal, parathyroid, and thyroid disease. It is brand new, very clean and there are no infectious disease patients or any other type of patients.
The first patient we had the honor of welcome is a 53-year-old lady from California. She, like many of our patients, experienced symptoms of an adrenal tumor for a long time before she was diagnosed. She was diagnosed initially with high blood pressure and atrial fibrillation. Atrial fibrillation is when your heart is skipping beats. An adrenal tumor is a very common underlying cause of atrial fibrillation.
Further work up revealed that she had a right adrenal mass and her laboratory tests proved that it was over-producing adrenaline-type hormones; catecholamines. This proves that she had a pheochromocytoma.
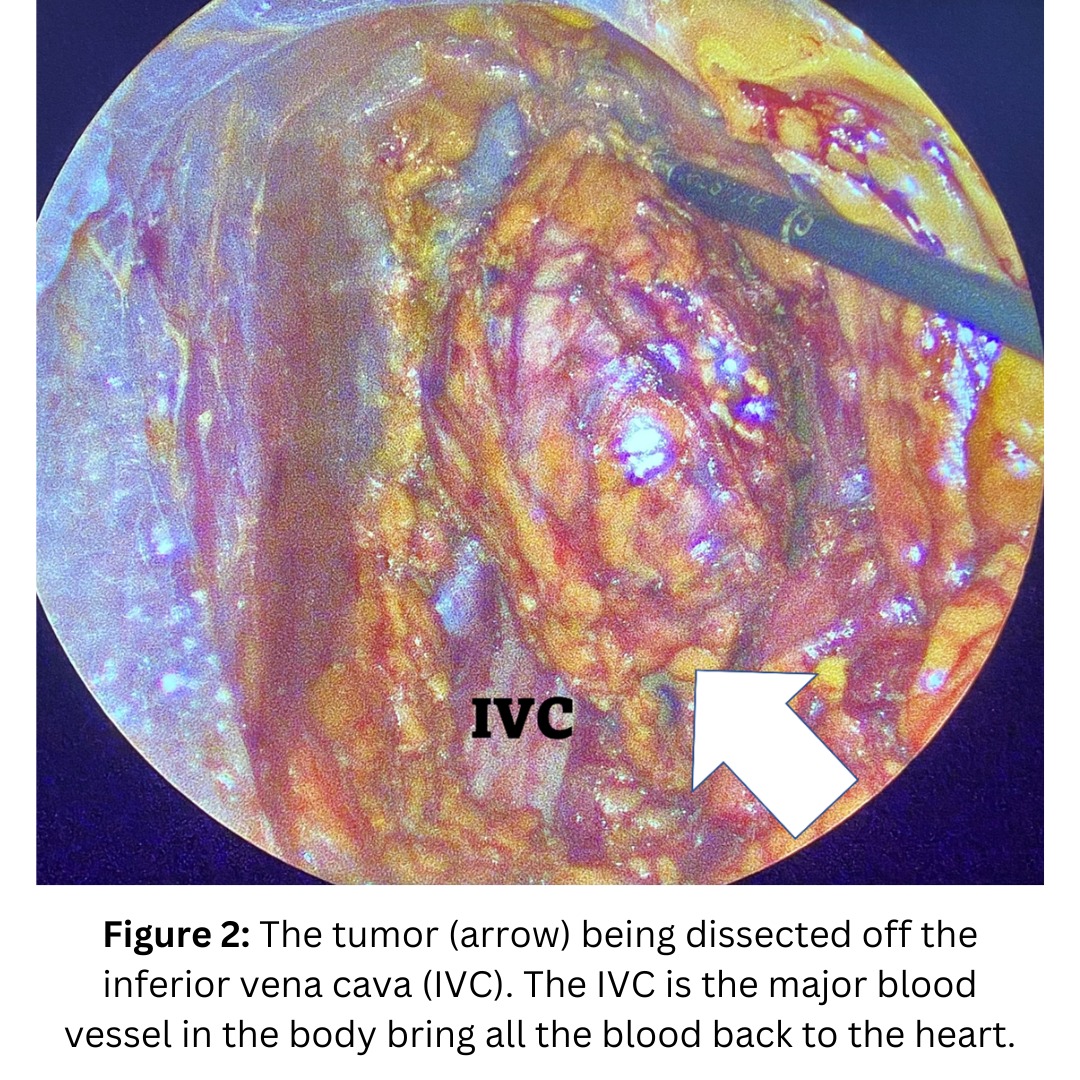
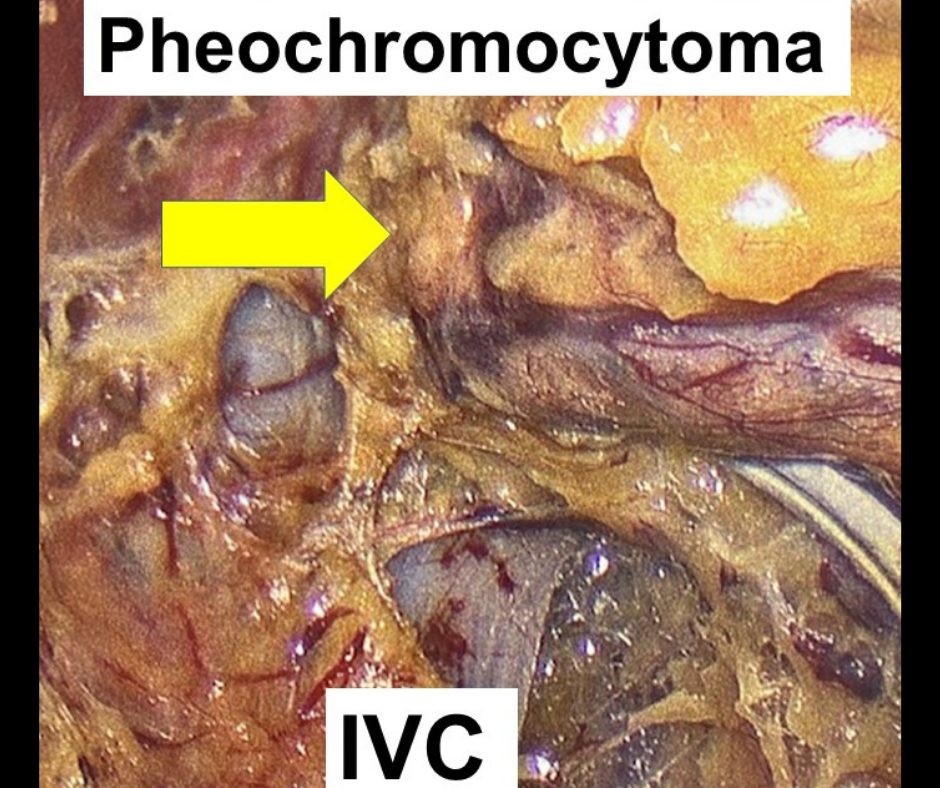
The photo below was taken with an endoscope, which is the type of camera Dr. Carling uses in the operating room. As you can see, he is peeling the pheochromocytoma off the inferior vena cava (IVC; the major vein in our body). As you can imagine, it requires superb skill to do this operation perfectly.
The patient did tremendously well! She is completely cured from her high blood pressure and could come off all her medication she was taking before the operation. She was able to leave the hospital first thing in the morning and is traveling back to California.
Become Dr. Carling's patient at the Hospital for Endocrine Surgery here.
Interesting case of the week: Patient with primary hyperaldosteronism (Conn’s syndrome) coming from Mississippi with Angel Flight Soars
The patient is a 51-year-old woman with primary hyperaldosteronism (Conn’s syndrome). This is due to an aldosterone-producing tumor of the adrenal gland. Her aldosterone level was high and her renin level low, proving primary hyperaldosteronism.
The patient was quite ill from this disease. In addition to high blood pressure heart palpitation and anxiety, she also had significant leg and arm cramps, as well as muscle weakness. Because of this she was not very mobile and one of her major concerns was how to be able to travel from Mississippi to Tampa for her adrenal operation.
Her CT scan shows a 2.2 cm right aldosterone-producing adrenal adenoma (yellow arrow).
Fortunately, our patient found out about a great volunteer organization that privately flies people throughout the Southeast for specialized medical treatment for free.
ANGEL FLIGHT SOARS is a volunteer pilot organization serving those who reside in, are traveling to or through the states of Georgia, Alabama, Mississippi, Tennessee, North Carolina and South Carolina.
Angel Flight Soars serves the community by coordinating free non-emergency air transportation to life-changing medical care that is not available locally, and for other compassionate purposes for the benefit of the community. They are dedicated to coordinating free flights on private aircraft with volunteer pilots and to working with the medical community to arrange these services for the community in need. The majority of their missions are flown in single- or twin-engine, four- to six-seat aircraft. www.AngelFlightSoars.org
Her pilot landed her in Tampa, and after undergoing a 19-minute right mini back scope adrenalectomy (MBSA) she was cured of her primary hyperaldosteronism.
Read more about the mini back scope adrenalectomy (MBSA) here.
The bad aldosterone-producing adrenal tumor is pictured here.
Interesting case of the week: Covid-19 infection leads to diagnosis and cure of pheochromocytoma
This week I saw a 51-year-old man from Illinois who developed a COVID-19 infection in September. He became relatively sick to the point where he required going to the emergency room where he was diagnosed with COVID-19 pneumonia.
They treated him with monoclonal antibodies, and he did well. Given that he had pneumonia, the ER doctors had performed a CT scan of his chest where they observed a 3 cm right adrenal mass.
Fortunately, his doctors did not ignore this mass, but referred him for a hormonal work up as well as a follow up MRI. The laboratory tests showed that he had slightly elevated 24-hour metanephrines. His normetanephrines as well as total metanephrines were about twice the upper limit. These findings are borderline when it comes to diagnosing pheochromocytoma. Most patients with pheochromocytoma have adrenaline-type hormone levels that are > 5 to 10 times normal. However, we certainly see patients with mild elevation as well. The follow up MRI demonstrated some features consistent with a pheochromocytoma.
He contacted us here at the Carling Adrenal Center and we swiftly reviewed all his information.
The right adrenal mass (yellow arrow) on the CT scan is shown in this picture. The white arrow indicates a normal left adrenal gland. Read more about imaging and X-ray studies of adrenal tumors here: https://www.adrenal.com/adrenal-tumors/scans
The patient underwent a 23-minute mini back scope adrenalectomy, and he did tremendously well.
Read more about the mini back scope adrenalectomy (MBSA) here.
The pathology did reveal a 3.5 x 3.0 x 2.7 cm right pheochromocytoma.
COVID-19 is a bad disease, but at least in this case it facilitated the early diagnosis of this patient’s pheochromocytoma. A swift surgical cure means that this patient will be spared all of the potentially catastrophic complications of undiagnosed pheochromocytoma.
Interesting case of the week: Fast growing adrenal tumor in a patient from Cameroon, Africa
Often the medical history, pathology or clinical presentation are unusual and interesting in our adrenal patients. Additionally, their lives and circumstances always fascinate me. Each patient has their own story, and it is always worth telling. Occasionally, patients come from the local Tampa Bay area, but more than 60% of our patients come from outside of Florida.
Due to the Covid-19 pandemic, it has been more challenging for our worldwide patients to fly into Tampa for the best possible adrenal surgery care. Nonetheless, some have been able to come, and as international travel is becoming more frequent again, so are our global patients.
The patient is a 55-year-old lady originally from the United Sates, but who currently lives and works in Cameroon, Africa. She did not have a lot of symptoms, and a CT scan (done for other reasons) in early January performed in Cameroon demonstrated a 3.6 cm partially calcified left adrenal tumor. The biochemical workup was unremarkable and showed no overt hormone overproduction.
Wisely, the patient was scheduled for a follow up imaging study, which now in September suggested that the tumor had grown to 5.8 cm. Interval growth and a tumor size over 4 cm are indications for surgery.
Read more about imaging and best X-ray studies of adrenal tumors here.
The patient flew in from Africa and underwent a 21-minute left mini back scope adrenalectomy (MBSA) for the left adrenal mass.
Fortunately, the pathology revealed a benign (non-cancerous) tumor, and the figure demonstrates the tumor with surrounding normal adrenal and fibroadipose tissue.
She was able to swiftly recover and return to her important work serving the people of Cameroon. We were honored to take care of her.
Read more about the mini back scope adrenalectomy (MBSA) here.
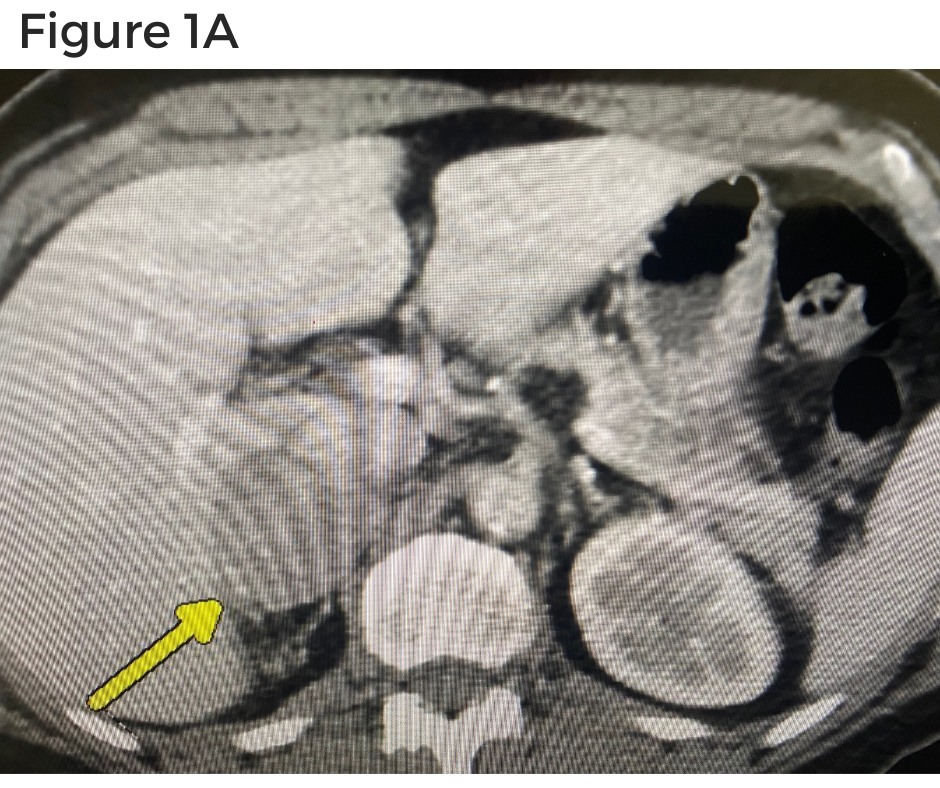
Interesting case of the week: What could be better? Getting two endocrine tumors fixed in one visit!
The patient is a 62-year-old lady from Austin, Texas. She did not have a lot of symptoms, but she did have high blood pressure. An MRI of her adrenals had demonstrated a 3.9 cm right adrenal tumor which the radiologist suggested could be concerning for adrenal cancer or possibly pheochromocytoma.
Her doctors correctly had checked her hormone levels and, indeed, her plasma free metanephrines and normetanephrines were all elevated. This clinches the diagnosis of pheochromocytoma. She was correctly placed on blood pressure control (alpha blocker) in preparation for surgery.
For some unfathomable reason, her doctors had talked to her about having a biopsy of the adrenal mass. Fortunately, the patient had read up on adrenal.com and called me before anybody could potentially put the needle into her adrenal mass. BIOPSY OF A PHEOCHROMOCYTOMA IS CONTRAINDICATED. Just don’t do it!
Doing a biopsy of an adrenal pheochromocytoma is not only completely useless but is potentially dangerous because it can release the adrenaline type hormones and lead to severe bleeding and a spike in the blood pressure resulting in stroke.
Learn more about the top 5 symptoms of pheochromocytoma.
You can review her Adrenal CT scan with contrast in figure 1A and figure 1B. The yellow arrow indicates the right adrenal pheochromocytoma.
Interestingly, the patient also had a large symptomatic left thyroid nodule. Anytime you have a thyroid nodule together with a pheochromocytoma you always need to keep medullary thyroid cancer and multiple endocrine neoplasia type 2 (MEN2) in the back of your mind. However, her calcitonin levels were normal which effectively rules out medullary thyroid cancer. Thus, her thyroid mass was likely just a benign thyroid goiter. However, she was sufficiently symptomatic with difficulty swallowing, choking as well as globus sensation.
You can review her thyroid ultrasound here in figure 2A and figure 2B. The yellow arrow indicates the large left thyroid nodule that is pushing on her windpipe (trachea) and food pipe (esophagus).
The patient flew down and on Tuesday underwent a 19-minute right mini back scope adrenalectomy (#MBSA) for her right adrenal pheochromocytoma. The patient did very well and spent one night in the hospital and Wednesday morning we took her back to the operating room and did a left thyroid lobectomy. The thyroid operation lasted two minutes longer.
The final pathology revealed a 4.6 cm pheochromocytoma completely resected and a 3.1 cm left thyroid follicular adenoma with no capsular or vascular invasion. EXCELLENT NEWS. The patient had curative resection of both her endocrine tumors and returned shortly to Texas and can put this all behind her.
So, what could be better? – Getting both her pheochromocytoma and thyroid follicular adenoma cured in one trip to beautiful Tampa, Florida.
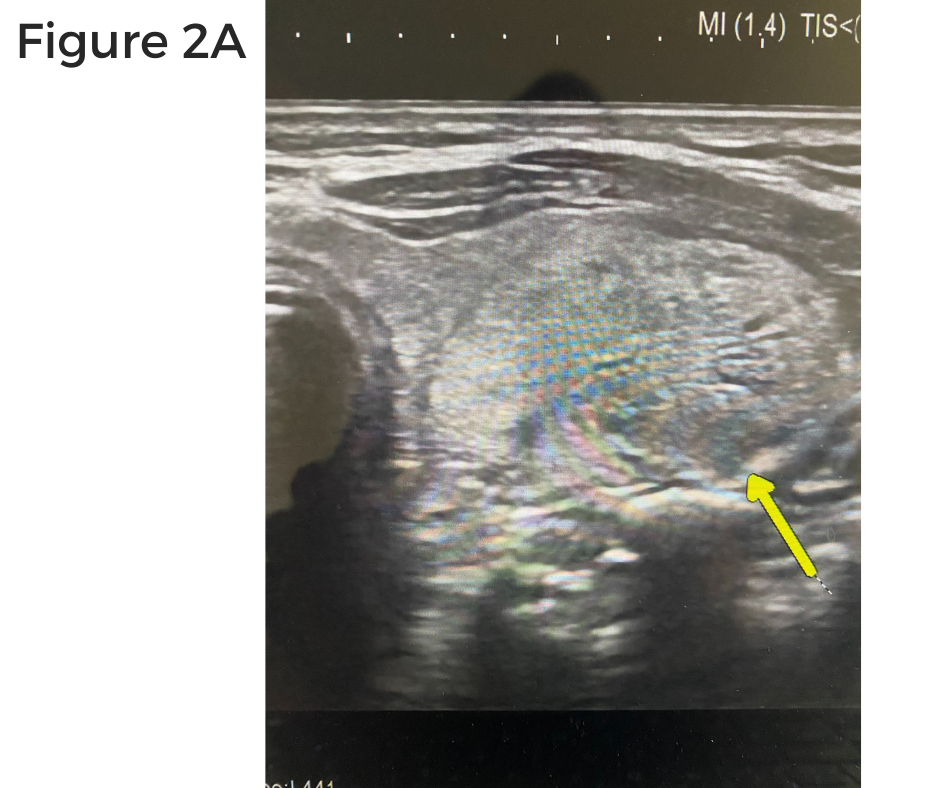
Interesting case of the week: Adrenal Cancer – No symptoms
The patient is a 69-year-old woman with an incidentally noted right adrenal tumor.
She had a CT scan back in September 2020 to evaluate a kidney cyst on the left side. The scan picked up on a nodularity on the right adrenal gland measuring 2.1 cm.
Fortunately, her doctors did not ignore her adrenal tumor. She was also sent to a medical endocrinologist who did a complete hormone work up. They made sure she did not have aldosterone-, cortisol-, or adrenaline- overproduction.
One year later they repeated the CT scan. Now the tumor had grown to 2.5 cm. On the CT scan there the tumor had an “atypical imaging phenotype”. This means that the tumor has some concerning features. The tumor was lipid-poor. This means that it does not have a lot of fat in it. This is a concerning sign.
At this point the patient was referred to me. When I reviewed all her scans, I was sufficiently concerned about this tumor that I recommended surgery. I recommended surgery even though the patient did not have any symptoms.
I review all the scans myself in great detail. I have looked at thousands of adrenal tumors on CT, PET and MRI scans. Her scan was concerning to me.
The patient underwent an uncomplicated right mini back scope adrenalectomy (MBSA). The operation lasted 21 minutes.
Two days later our specialist adrenal pathologist called me. Indeed, the suspicion I had about the scans was verified. The patient had an adrenocortical cancer (also known simple as adrenal cancer, or ACC).
Fortunately, because it was detected early it was still Stage 1. Importantly, all the margins were negative. This means the cancer was completely removed. It is likely that the patient will have a surgical cure and do very well.
We have already set up a team of doctors who will keep a very close eye on her for many years to come.
Interesting case of the week: Subclinical Cushing’s Syndrome patient didn't know just how bad she felt until after curative adrenal surgery
The patient is a 61-year-old woman with a cortisol-producing right adrenal tumor causing subclinical Cushing’s syndrome.
Patients with subclinical Cushing’s syndrome have too much cortisol and can suffer from many signs and symptoms.
Heartburn, heart palpitations, muscle weakness, decreased sex drive, difficulty concentrating, anxiety, problems with memory, and Irritability are common symptoms of Cushing’s syndrome.
Patients can gain weight, especially on the mid-section, and their back, so called 'buffalo hump', and often develop diabetes.
Easy bruising, poor wound healing, hair loss, and sleep apnea are other symptoms of too much cortisol.
The tricky thing with subclinical Cushing’s syndrome is that the symptoms often sneak up on the patient over months and years. Many patients don’t even realize how bad they feel because they attribute their symptoms to getting older. Sometimes, they do not realize how bad they really feel until the adrenal tumor is removed.
This patient had an incidentally identified adrenal tumor on a CT scan for another reason. Fortunately, her doctors did not ignore the tumor. They ordered appropriate lab test. She had a low (suppressed) ACTH level, and a cortisol level over 1.8 following a low dose dexamethasone suppression test. This proves adrenal subclinical Cushing’s syndrome.
The patient had a Mini Back Scope Adrenalectomy and did very well. She did not require steroids after the operation.
6 weeks later the patient contacted me and said she felt better than she had done in decades. Her energy level improved, and the brain fog was gone. She had already lost 7 lbs., and her blood sugars normalized to the point where she was no longer pre-diabetic. She was thrilled to get rid of the toxic effects of too much cortisol. She wished she had gotten rid of her adrenal tumor a long time ago.
Interesting case of the week: Adrenal Metastasis from Uterine Cancer with Dr. Tobias Carling
This week, I had the honor of operating on a 59-year-old woman with an unfortunate history of stage 4 cancer arising from her uterus.
She had undergone massive surgery with removal of her uterus, ovaries as well as other organs in her pelvis. She had done quite well for some time but follow-up scans showed a large mass on her left adrenal gland.
Additional scans showed no other evidence of metastasis (meaning spread of the cancer) except to the left adrenal gland. Whenever there is an isolated metastasis to the adrenal gland, surgery is recommended.
She traveled from the Midwest to the Carling Adrenal Center in Tampa to have her surgery. Review her CT scan with me here, showing a large left adrenal mass as well as what the mass looks like after it was removed.
The patient had a Mini Back Scope Adrenalectomy, and even though the tumor was very large (9 cm, Fig 1), the operation took less than 30 minutes. The patient very much benefited from having surgery through the back as supposed to through the abdomen. Having the Mini Back Scope Adrenalectomy meant that we could avoid all the scar tissue from her previous cancer operation of her uterine cancer.
She flew back home a couple of days later and will continue to be closely followed by her local oncologist.
Interesting case of the week: A young man with a rare adrenal tumor, with Dr. Tobias Carling
Adrenal masses in young patients should always be taken very seriously. In young patients, the risk of it being cancerous or hormone-producing is much higher than in older people.
This is a patient from Louisiana. He is very young, in his early 20s, and had undergone a CT scan of his abdomen. The scan was performed for other reasons but there was a finding of an incidental large left adrenal mass.
It measured 5.3 cm (greater than 2 inches) and it had some characteristics on the scan that was atypical or indeterminate. The patient did not have any symptoms but of course we measured all his hormone levels (cortisol, aldosterone, and adrenaline-type hormones) which were all negative.
As you know, one should almost never perform a biopsy of an adrenal tumor so clearly this tumor needed to come out.
He came down here for his operation and had a very straightforward left Mini-Back Scope Adrenalectomy (MBSA)
Our expert endocrine pathologist called within two days and gave me the very good news. This was a benign adrenal ganglioneuroma. Ganglioneuromas of the adrenal gland are rare. In the photo placed at the end of the video, you can see how the tumor arises just adjacent to the normal adrenal gland. These tumors are all benign, meaning not cancerous, and he is completely cured.
He will live a perfectly normal life and will never have to worry about this again.
Interesting case of the week: Texas Doctor with Primary Hyperaldosteronism (Conn’s syndrome) and a negative CT scan
High blood pressure, low potassium, fatigue, and muscle cramps occur in many patients with Primary Hyperaldosteronism also known as Conn’s syndrome.
The cause of Primary Hyperaldosteronism often is a small adrenal tumor that overproduce aldosterone. Too much aldosterone is very toxic for the body.
This patient is a doctor herself in Texas and in her early 40s. She is otherwise super-healthy and did not have any real for having high blood pressure. She had classical Conn’s syndrome.
She had a CT scan that did not show an obvious adrenal tumor. Fortunately, she was smart and so was her doctor, so they did not give up on her.
She underwent adrenal vein sampling, which directly measure the aldosterone production from each adrenal gland. This clearly proved that the left adrenal gland had a tumor.
She underwent a swift Mini Back Scope Adrenalectomy (MBSA).
Now the patient is cured of her primary hyperaldosteronism and Conn’s syndrome and is doing fantastically.
So, remember, even if the tumor does not show up on a CT or MRI, that does not mean you do not the disease. It just means that the tumor is not large enough to be picked up on a regular scan.
Interesting case of the week: This week, you'll hear directly from a young patient suffering with Cushing's Disease
Cortisol production by the adrenal glands is normally under the control of the pituitary (a small endocrine gland located in the bran right behind your eye). When a pituitary tumor secretes too much ACTH (adrenocorticotropic hormone), it causes the otherwise normal adrenal glands to produce too much cortisol. This type of
Cushing's syndrome is termed Cushing's disease.
The treatment for this is pituitary surgery to remove the tumor. When pituitary surgery works (70%), it is great! However, about 1/3 will never be cured in the fist place or the tumor grows back (recurrence). This is a BIG problem.
In these patients removing all cortisol-producing cells, meaning bilateral adrenalectomy is often the best option. The goal is to remove all cells in the adrenal glands overproducing the toxic cortisol.
Many recent studies have shown that bilateral adrenalectomy is an increasingly used and essential treatment option when pituitary surgery is no longer an option. Compared to other options such as radiation or medical treatment, bilateral adrenalectomy lowers morbidity and mortality rates, as well as improves quality-of-life.
Again, the Mini-Back Scope Operation (MBSA) is the best adrenal operation for “failed” ACTH-dependent Cushing’s syndrome, Cushing’s Disease. Do not go through the tummy to get to the adrenal glands!
Interesting case of the week: Bilateral Cushing's syndrome
The symptoms of adrenal pheochromocytoma can be variable, and often missed by doctors for years and decades. Check out the top 5 symptoms of pheochromocytoma.
All symptoms of a pheochromocytoma are due to the very toxic effects of too much adrenaline hormones (catecholamines).
Symptoms from a pheochromocytoma are often characterized by “spells”. This means patients develop symptoms from the pheo during an attack, a “spell”, which often last 5 to 20 minutes. The typical spell is associated with very high blood, headache, palpitations (heart racing), and sweating. Chest or belly pain is also common
However, not all patients with pheochromocytoma have symptoms. As many as 30% of pheochromocytoma patients have no symptoms.
Let me introduce you to a very pleasant female patient of mine.
She is 77 years old, but strong as an Ox. She still works her farm, from sunrise to late into the evening.
Indeed, sometimes I had difficulty tracking her down because she was running around the farm on her tractor. At 77 years old. She is one tough Florida lady.
She felt fine. She felt strong. The only problem she had was high blood pressure.
She did have a CT scan though for other reasons, and this showed a 2.3 cm right adrenal tumor (see Figure 1).
This tumor did not look like a typical innocent benign (non-cancerous) adenoma, so her doctor ordered a PET scan, which also showed some concerning features (review video of her CT scan here: https://youtu.be/Wx0VpahVVLw).
Clearly, she needed surgery. We did measure her adrenaline hormones (Catecholamines, Metanephrines), and they were only slightly elevated.
I performed a 16 minute Right Mini Back Scope Adrenalectomy (MBSA). I almost always can tell in the operating room when I look at the tumor, I can tell what it is, and I knew instantly that it was a pheochromocytoma (see Figure 2). She did awesome!
My sweet 77-year-old famer lady did great and was back on her tractor working within a couple of days.
So, remember, not all pheochromocytoma patients have symptoms!
Interesting case of the week 9/17/2021: Right pheochromocytoma, no symptoms with Dr. Tobias Carling
Interesting case of the week: Bilateral Cushing's syndrome
Cushing’s syndrome or too much cortisol is probably the one disease that confuse the most doctors, nurses and patients. But when it comes to adrenal Cushing’s syndrome, it is actually quite straightforward. Adrenal Cushing’s syndrome means too much cortisol that originates from the adrenal gland. This is either from one adrenal tumor or from both adrenal glands, called bilateral adrenal Cushing’s syndrome.
Another name for Cushing’s syndrome due to masses of the adrenal glands is ACTH-independent Cushing’s syndrome. This differentiates it from Cushing’s Disease which is ACTH-dependent. The problem then is a tumor in the pituitary gland of the brain overproducing ACTH.
To diagnose Cushing’s syndrome, lab tests prove that the patient have too much cortisol production. This can be done through a number of tests including the low-dose dexamethasone suppression test, a salivary cortisol test, or a 24-hour urine collection for cortisol. If the ACTH level (which is the pituitary hormone that controls the adrenal) is on the low side or frankly suppressed that proves that the problem originates in the adrenal glands.
The patient is a doctor from Southern California. He has for many years had adrenal Cushing’s syndrome. His ACTH level has always been low, but his cortisol level has been high. This has been proven multiple times through 24-hour urine collection and low dose dexamethasone suppression test.
He had many very difficult symptoms with muscle weakness, decreased sex drive, problems with concentration and memory, anxiety, low potassium, high blood pressure. He was required to take multiple medications including blood pressure medication and extra potassium although otherwise, he was a very fit and healthy person. All these symptoms affected his quality of life and his work as a doctor.
His doctor had started him on a medication called Korlym. Korlym is a drug that blocks the cortisol effect. This medication does not fix the problem. It is not a cure for Cushing’s syndrome. It does not remove the tumors in the adrenal glands.
However, sometimes it can treat the symptoms and make life a little bit more bearable for the patients until they can have surgery and get cured of the disease.
So, he was started on Korlym until he could come to me in Tampa for his adrenal gland removal.
A couple of months ago, I performed bilateral cortex-sparing adrenalectomy on him. This was done by the Mini Back Scope Adrenalectomy (MBSA) approach. I removed almost all adrenal tissue except leaving about 30 to 50% of one adrenal gland. This is because he had bilateral tumors, meaning tumors on both the right side and the left side. This left the perfect amount of adrenal tissue such that he was cured of his Cushing’s syndrome, but also has enough cortisol production that he does not need to take long-term steroid hormone supplementation. This is a “Goldilocks” operation, meaning the amount of adrenal tissue remaining is “just right”.
Now the patient is cured of his Cushing’s syndrome and is doing very well. He required a short period of time (a few weeks) to take supplementary cortisol (Prednisone) until the remnant adrenal gland tissue produced enough cortisol by itself.
Interesting case of the week: When radiologists miss adrenal tumors
I love radiologists.
In fact, my younger brother and my best friend from medical school are both radiologists. But radiologists sometimes miss things, and this is especially true when it comes to #adrenaltumors. In particular, small aldosterone producing #adrenaladenomas can easily be missed.
These small adrenal adenomas that overproduce aldosterone cause primary #hyperaldosteronism or #ConnsSyndrome.
Often these aldosterone-producing adrenal tumors are quite small, less than half an inch or about one centimeter. The is the size of a pea or a small grape.
Why do radiologists miss small adrenal tumors on CT scans?
Radiologists look at hundreds of CT scans in a single day. They look at dozens and dozens of different organs in your body. When a radiologist looks at the CT scan of the chest and abdomen, they review the lungs, heart, liver, kidneys, spleen, pancreas, bowels, and all sorts of different organs. A small adrenal tumor can easily be missed.
The patient in her mid-fifties from the Mountain West had high blood pressure for decades. She was not overweight, diabetic or had any real reasons for having high blood pressure. Despite this, she required 4 blood pressure medications including Spironolactone.
Her aldosterone level was very high and her renin level very low (suppressed). She also had problems with too low potassium. She had a potassium as low as 2.4 once. This is dangerously low. She was a “slam-dunk Aldo”. This means it is so obvious that a 3rd year medical student should be able to diagnose it.
However, on the scan of her adrenals, the report stated that the adrenal glands were normal.
When I reviewed her CT scan, she had on obvious left adrenal tumor, measuring 13 mm.
Figure 1 and 2 shows the aldosterone-producing adrenal adenoma on the CT scan and after it was removed by a 19-minute Mini Back Scope Adrenalectomy (MBSA).
Now the patient is cured of her primary hyperaldosteronism and Conn’s syndrome and is doing fantastically.
So, remember, it is very important that the radiologist knows that you have an adrenal problem, and that they scrutinize the adrenal gland on the scan very carefully.
Interesting case of the week: Adrenal Metastasis
This week, I saw a patient with cancer that had spread to the adrenal gland. This is called adrenal metastasis and occurs most commonly with breast, lung, kidney, colon, rectal, and stomach cancers as well as malignant melanoma. Adrenal surgery is used to treat and sometimes cure cancer which has spread to the adrenal gland. This is advanced surgery and should only be performed by the most experienced adrenal surgeons. You also need your surgeons to be experienced to scrutinize your scans (CT, MRI, PET, etc).
Prior to seeing me, this patient had undergone significant treatment for his kidney cancer. They had already removed his right kidney which contained the original cancer and he was told they removed the left adrenal gland because the cancer had spread.
His cancer had come back in his right adrenal gland and required surgery. He was now facing a dilemma and was told by his doctors that he could have the right adrenal gland removed but would need to take medication for the rest of his life.
When I looked at his scan, I determined his left adrenal gland wasn't actually removed during the original surgery. Watch the video to learn more!