What X-Rays and Scans are Best for Adrenal Tumors?
There are 4 primary radiological (x-ray) tests to examine the adrenal glands (and the rest of the abdomen) for the presence of a tumor (the word "tumor" simply means "mass". These can be benign or malignant). Some of these tests are better than others and are therefore used routinely, while one or two are used infrequently yet can yield important information when positive.
 Dr. Carling meticulously studies a CT scan prior to a Mini Back Scope Adrenalectomy (MBSA) operation. Dr. Carling has reviewed thousands of adrenal tumor scans.
Dr. Carling meticulously studies a CT scan prior to a Mini Back Scope Adrenalectomy (MBSA) operation. Dr. Carling has reviewed thousands of adrenal tumor scans.
When we look at the imaging of the adrenal gland whether it is an ultrasound, CT, MRI, nuclear medicine (MIBG, PET, etc) scan or other imaging study, we need to have a whole-person approach and evaluate all aspects of the tumor and the patient. We carefully analyze the "imaging phenotype" of the tumor. The "imaging phenotype" describes all aspects of what the tumor looks like on your scan and helps us arrive at the correct diagnosis, including the likelihood of cancer. It should be noted, this is far from a perfect science. In many cases we can never know for sure whether the tumor is cancerous short of removing it via adrenalectomy. Since the interpretation of adrenal imaging is not black and white, you need a team and a surgeon who is experienced and has great judgment.
What do the expert adrenal doctors look for on the adrenal x-rays and scans? What we look for on an imaging study (scan) is a combination of more than a dozen criteria giving us a total impression, called the "imaging phenotype". For instance, we carefully examine the size and the shape of the tumor. That means we will look at whether the borders are smooth or irregular, whether the margins are clear or unclear, and so forth.
The key and most important points of adrenal imaging and adrenal scanning are:
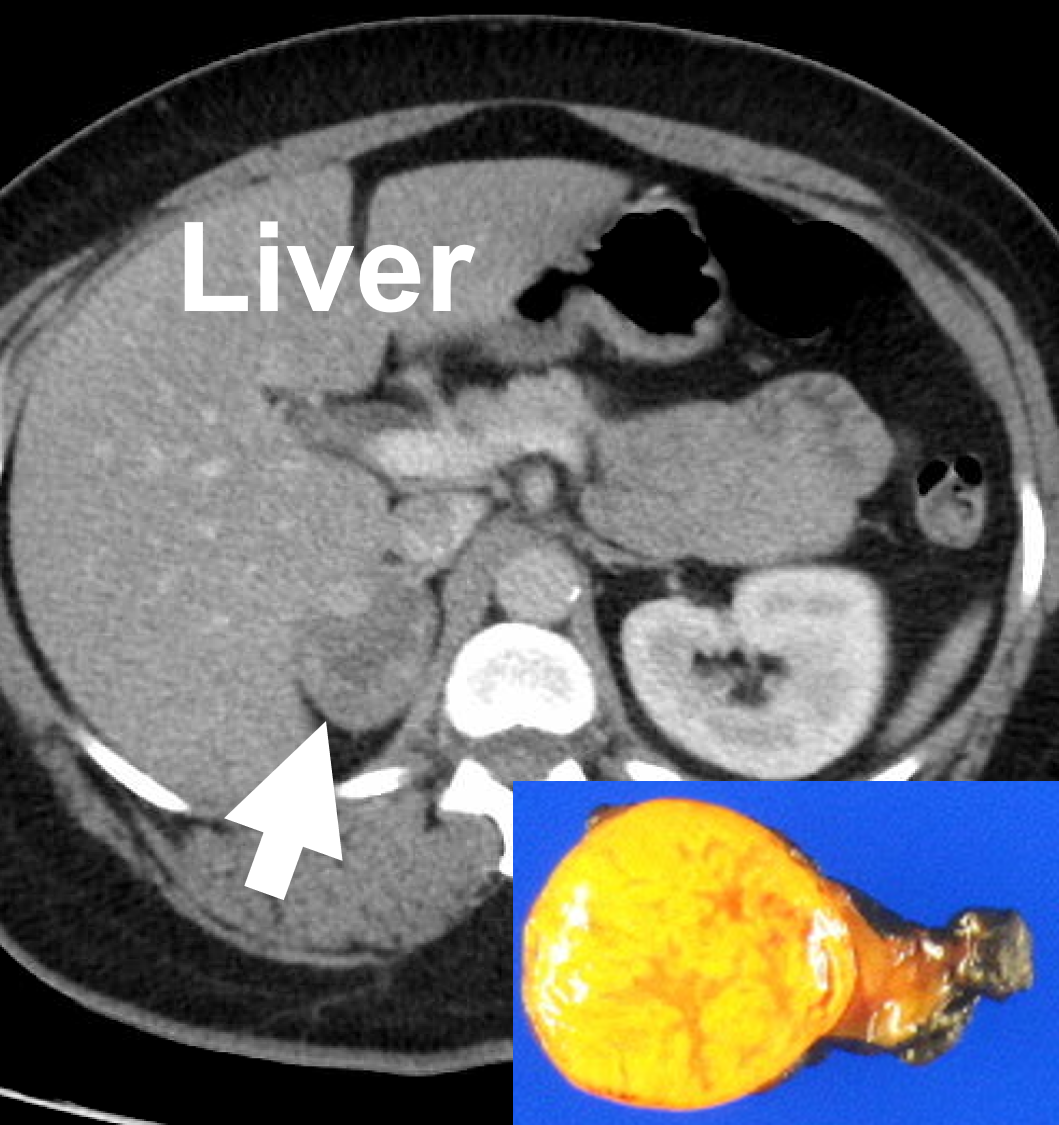 Adrenal protocol, contrast-enhanced CT scan demonstrating a right adrenal adenoma (4.4. cm, arrow), causing Cushing's syndrome. Benign adrenal adenomas are typically smooth, round or oval, homogeneous and lipid-rich.
Adrenal protocol, contrast-enhanced CT scan demonstrating a right adrenal adenoma (4.4. cm, arrow), causing Cushing's syndrome. Benign adrenal adenomas are typically smooth, round or oval, homogeneous and lipid-rich.
- A benign cortical adenoma is the most common adrenal tumor and it is almost always round. A cortical adenoma is an adrenal tumor that grows from the adrenal cortex -- the outermost layer of the adrenal gland. (See adrenal anatomy for more information)
- The gold standard of adrenal imaging is a CT scan (CAT scan). An “adrenal-protocol, contrast enhancement CT scan” is best. Thus, a CT scan of the adrenal with and without contrast should always be the first scan ordered, and in more than 90% of cases, the ONLY scan a patient will need. The exception to this rule is that if you have an allergy to contrast dye, then obtain a CT scan without contrast.
- MRI scans are almost never necessary and should never be the first scan that a doctor orders to look at adrenal masses.
- Nuclear medicine scans are almost never necessary. Nuclear medicine scans is helpful in some very specific settings that few doctors will ever see.
- Ultrasound is not very helpful, so don't bother.
CT Scans (CAT Scans) to Evaluate Adrenal Tumors and Growths
The CT scan (also called CAT scan) is very accurate at examining the adrenal glands and other abdominal structures and can be used on any type of adrenal tumor. Like the other 3 tests in this group, the CT scan is painless. It will take only a few minutes to complete. The pictures which result are very good at demonstrating tumors throughout the body and very accurate measurements can be taken, which help the planning of subsequent therapies. CT represents the first-level imaging modality for the evaluation of adrenal lesions since it fast, ensures great resolution, with findings of pre-contrast images and post-contrast behavior being commonly used to achieve a correct diagnosis.The “adrenal protocol, contrast-enhanced CT scan” is the best scan or x-ray for adrenal tumors and masses. An unenhanced (no IV contrast is given to the patient) is good, but not nearly as good as a CT with IV contrast. On CT scans, adrenal adenomas are usually well-demarcated round or oval lesions, with homogeneous and relatively low attenuation values (lower than 10 Hounsfield Units [HU]), due to high fat content. Unfortnuately, unenhanced (non-contrast) CT alone is not always diagnostic since 15–30% of adenomas are lipid-poor, thereby showing higher attenuation values. In these cases, additional imaging after intravenous contrast administration (adrenal protocol, contrast-enhancement CT scan) is required to differentiate adenomas from non-adenomas. The evaluation of the enhancement pattern of adrenal lesions needs a further late phase after the venous phase. There are different CT protocols suggested for the evaluation of adrenal masses; however, there is evidence that a 15-min post-contrast protocol has best diagnostic accuracy.
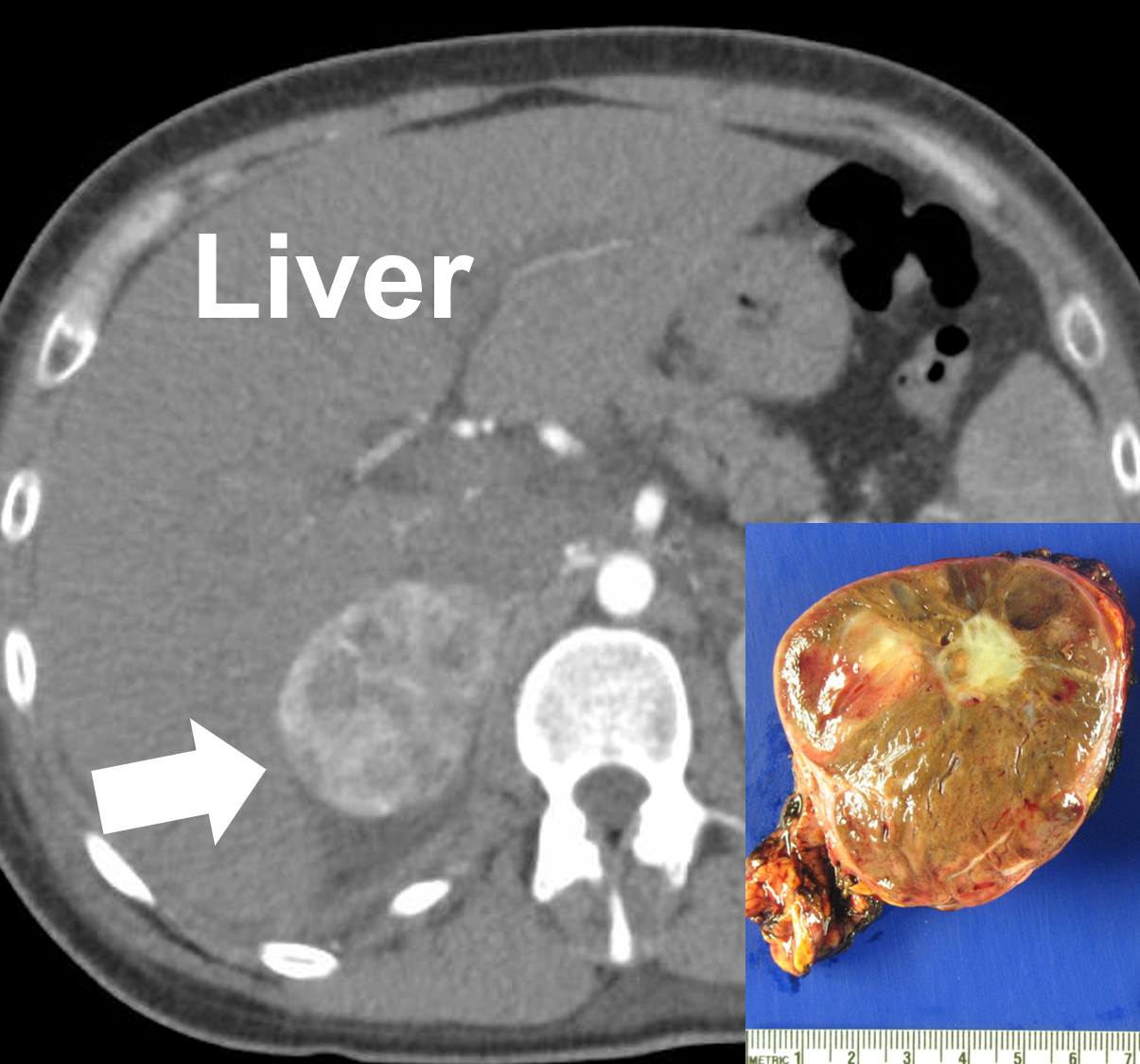 A right 6 cm pheochromocytoma seen on a CT scan (arrow) and after removal. Pheochromocytomas are vascular and may appear variable with solid, cystic, calcified, and necrotic components.
Sorry folks for the technical stuff, This is by far the most technical page of this huge website. We do this because almost every endocrinologist that gets a patient with an adrenal tumor reads this website, so we must throw in some technical stuff for them so they can take better care of you. Don't worry about the technical stuff if you are not a doctor -- keep reading because 95% of this website is written for patients as well as doctors.
A right 6 cm pheochromocytoma seen on a CT scan (arrow) and after removal. Pheochromocytomas are vascular and may appear variable with solid, cystic, calcified, and necrotic components.
Sorry folks for the technical stuff, This is by far the most technical page of this huge website. We do this because almost every endocrinologist that gets a patient with an adrenal tumor reads this website, so we must throw in some technical stuff for them so they can take better care of you. Don't worry about the technical stuff if you are not a doctor -- keep reading because 95% of this website is written for patients as well as doctors.
The absolute percentage washout (APW) of contrast from the adrenal tumor can then be calculated using a formula. The relative percentage washout (RPW) is used when unenhanced CT value is not available. If the APW is >60% or RPW is >40% after 15-min from contrast administration, this is indicative of benign adenoma, with sensitivity and specificity of 88% and 96% at the APW and sensitivity and specificity of 83% and 93% at the RPW, respectively.
This method can to some degree of certainty differentiate benign adenomas, which enhance quickly and show rapid washout, from non-adenomas such as adrenocortical cancer, pheochromocytomas and metastases, which instead demonstrate strong enhancement but prolonged washout.
Pheochromocytomas on Contrast-Enhanced CT Scans. Pheochromocytomas can present with solid, cystic, calcific, and/or necrotic components--quite variable. Smaller pheos tend to display a more uniform attenuation, with a density of 40–50 HU. After contrast administration, pheochromocytomas enhance avidly (meaning turn very bright) with some of them showing higher enhancement on the portal venous phase and others on the arterial phase; nevertheless, their APW and RPW are similar to those of adenomas. Therefore, pheochromocytomas often cannot be reliably differentiated from adenomas using CT washout protocols. When lesions are quite large (>6 cm), intralesional hemorrhage, necrosis, or calcifications can be observed.
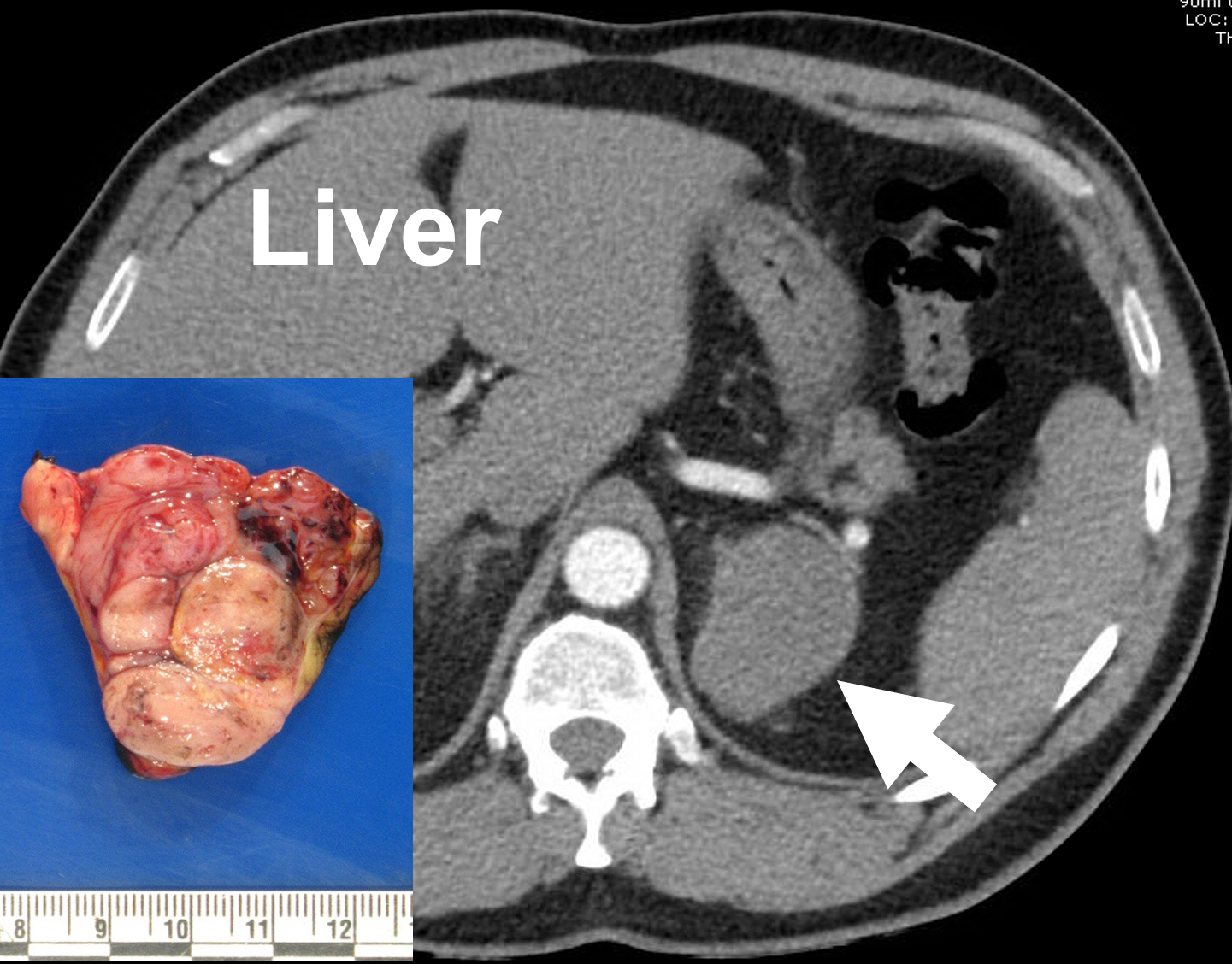 A left adrenocortical cancer (arrow) depicted on an adrenal protocol (arterial phase) contrast-enhanced CT, and following removal. Adrenal cancers often display a heterogeneous (variable) appearance due to necrosis, calcifications, and bleeding into the tumor.
A left adrenocortical cancer (arrow) depicted on an adrenal protocol (arterial phase) contrast-enhanced CT, and following removal. Adrenal cancers often display a heterogeneous (variable) appearance due to necrosis, calcifications, and bleeding into the tumor.
Metastasis to the adrenal gland (most commonly carcinomas of the lung, breast, kidney, and melanoma) appear as focal masses with strong and prolonged enhancement on the portal venous phase, usually more than 120 HU, but slower washout than adenomas. It should be noted that the appearance of adrenal metastasis can be very variable depending on the underlying cancer.
MRI Scans to Evaluate Adrenal Tumors
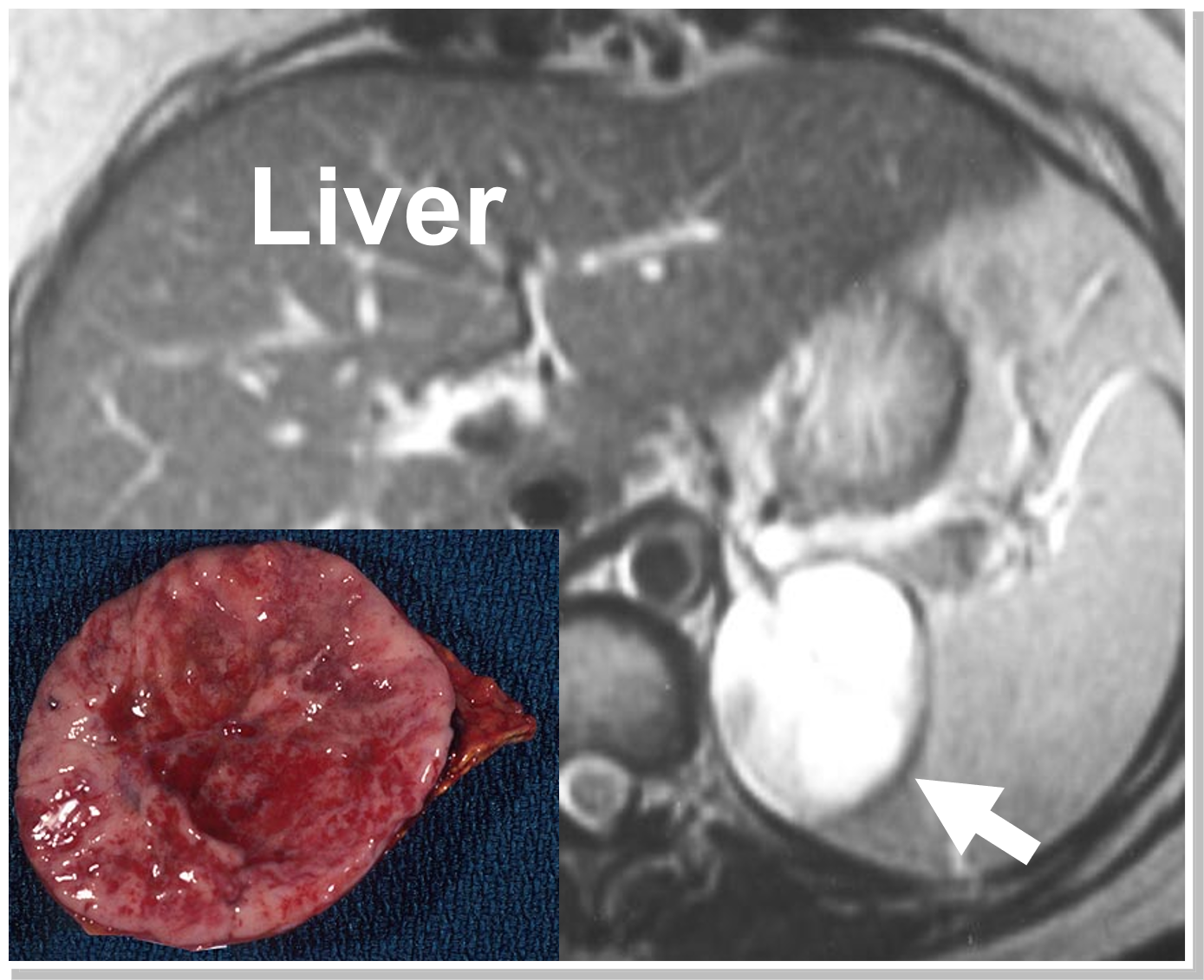 An MRI demonstrating a left pheochromocytoma (arrow and pathology). Often pheochromocytomas enhance (light up brightly) on an MRI scan which is so characteristic that it by itself clinches the diagnosis.
An MRI demonstrating a left pheochromocytoma (arrow and pathology). Often pheochromocytomas enhance (light up brightly) on an MRI scan which is so characteristic that it by itself clinches the diagnosis.
The MRI (also called an MR scan or NMR scan) is very similar to the CT scan in the type of information and pictures it provides. The scan takes about an hour and uses magnetic fields to generate pictures of body structures rather than x-rays like the CT scan or sound waves like the ultrasound.
MRI has similar diagnostic accuracy to CT, allowing characterizing adenomas regardless of their CT enhancement. On T2-weighted MR images (fluid-filled tissues appear bright), adrenal adenomas are homogeneous and present intermediate-low signal intensity compared to skeletal muscle or liver. An important component of adrenal MRI protocol is chemical shift imaging (CSI). This modality enables the radiologist to detect intra-tumor fat resulting in a loss of signal intensity. The MR sensitivity for adenomas measuring 10–20 HU is nearly 100%, while that for lipid-poor adenomas measuring greater than 30 HU is significantly lower (13–75%)Often pheochromocytomas enhance (light up brightly) on an MRI scan which is so characteristic that it by itself clinches the diagnosis. Of course, pheochromocytoma patients still need to have their plasma and urine (24 hour collection) measurements of fractionated metanephrines and catecholamines measured and be appropriately prepared prior to adrenalectomy.
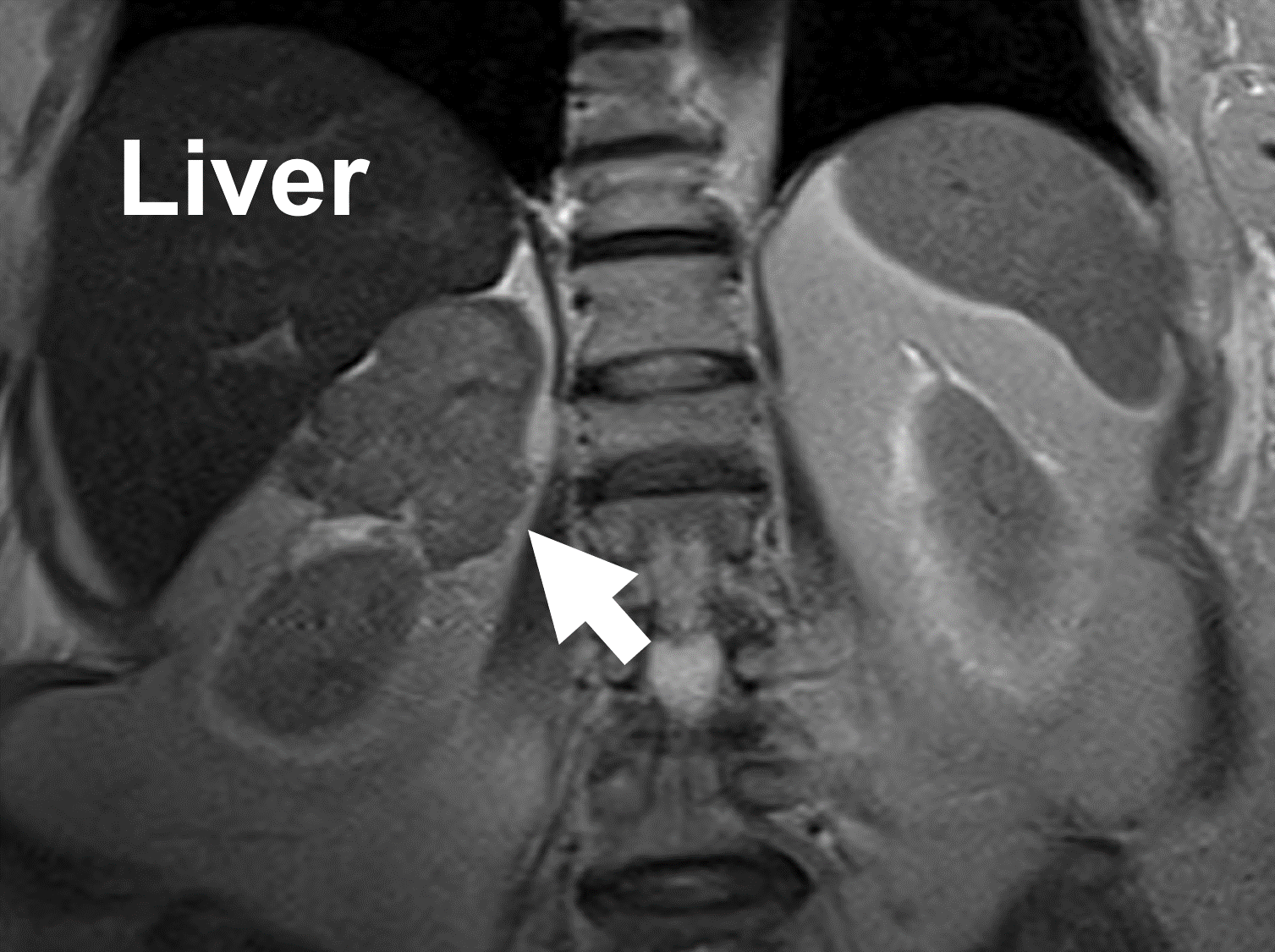 MRI showing an adrenal cancer (arrow) arising from the right adrenal gland. Note the heterogeneity and irregular borders.
On MR, adrenocortical carcinomas show low signal intensity on T1-weighted images, high signal on T2-weighted images, and strong and heterogeneous contrast enhancement with slow washout. Similarly, metastasis to the adrenal gland can appear very variable on an MRI scan.
MRI showing an adrenal cancer (arrow) arising from the right adrenal gland. Note the heterogeneity and irregular borders.
On MR, adrenocortical carcinomas show low signal intensity on T1-weighted images, high signal on T2-weighted images, and strong and heterogeneous contrast enhancement with slow washout. Similarly, metastasis to the adrenal gland can appear very variable on an MRI scan.
Are Nuclear Medicine Scans Useful For Evaluating Adrenal Tumors?
A nuclear medicine scan uses radioactive substances (a very low radiation dose) to take pictures of areas inside the body. The radioactive substance is injected into the body, and locates and binds to specific cells or tissues, including cancer cells. The technology is similar to a radioactive iodine scan used in thyroid disease, or a sestamibi scan used in parathyroid disease.
A nuclear medicine scan is only needed for certain cases of adrenal tumors, when CT and MRI scans are not sufficient. The most commonly used nuclear imaging scans in adrenal tumor imaging are:
- MIBG (I-131 MIBG)
- DOTATATE PET (Gallium-68 PET/CT)
- Regular PET (18-FDG-PET/CT)
 An MIBG scan demonstrating positive uptake in the right adrenal gland (arrow) proving to be a pheochromocytoma.
The MIBG scan is used only to detect the presence and location of pheochromocytomas and paragangliomas (also known as extra-adrenal pheochromocytomas). This test does NOT detect any other type of adrenal tumor. MIBG is another nuclear medicine scan which takes advantage of the fact that endocrine cells make hormones. A special radioactive dye is given to a patient which is a precursor for adrenaline (the hormone made by the adrenal medulla). This dye is concentrated in the hyperactive endocrine tissue which comprises the pheo and it can be seen on x-ray film. MIBG scintigraphy is the functional nuclear medicine imaging of choice for pheochromocytoma and paraganglioma, but suffers from drawbacks like limited spatial resolution, difficulty in detection of small tumors (< 1.5–2.0 cm) or large tumors with extensive necrosis/ hemorrhage, lack of tracer uptake in some tumors, and interference with certain medications, leading to false-negative results.
An MIBG scan demonstrating positive uptake in the right adrenal gland (arrow) proving to be a pheochromocytoma.
The MIBG scan is used only to detect the presence and location of pheochromocytomas and paragangliomas (also known as extra-adrenal pheochromocytomas). This test does NOT detect any other type of adrenal tumor. MIBG is another nuclear medicine scan which takes advantage of the fact that endocrine cells make hormones. A special radioactive dye is given to a patient which is a precursor for adrenaline (the hormone made by the adrenal medulla). This dye is concentrated in the hyperactive endocrine tissue which comprises the pheo and it can be seen on x-ray film. MIBG scintigraphy is the functional nuclear medicine imaging of choice for pheochromocytoma and paraganglioma, but suffers from drawbacks like limited spatial resolution, difficulty in detection of small tumors (< 1.5–2.0 cm) or large tumors with extensive necrosis/ hemorrhage, lack of tracer uptake in some tumors, and interference with certain medications, leading to false-negative results.
What PET Scans are Used to Evaluate Adrenal Tumors and Growths?
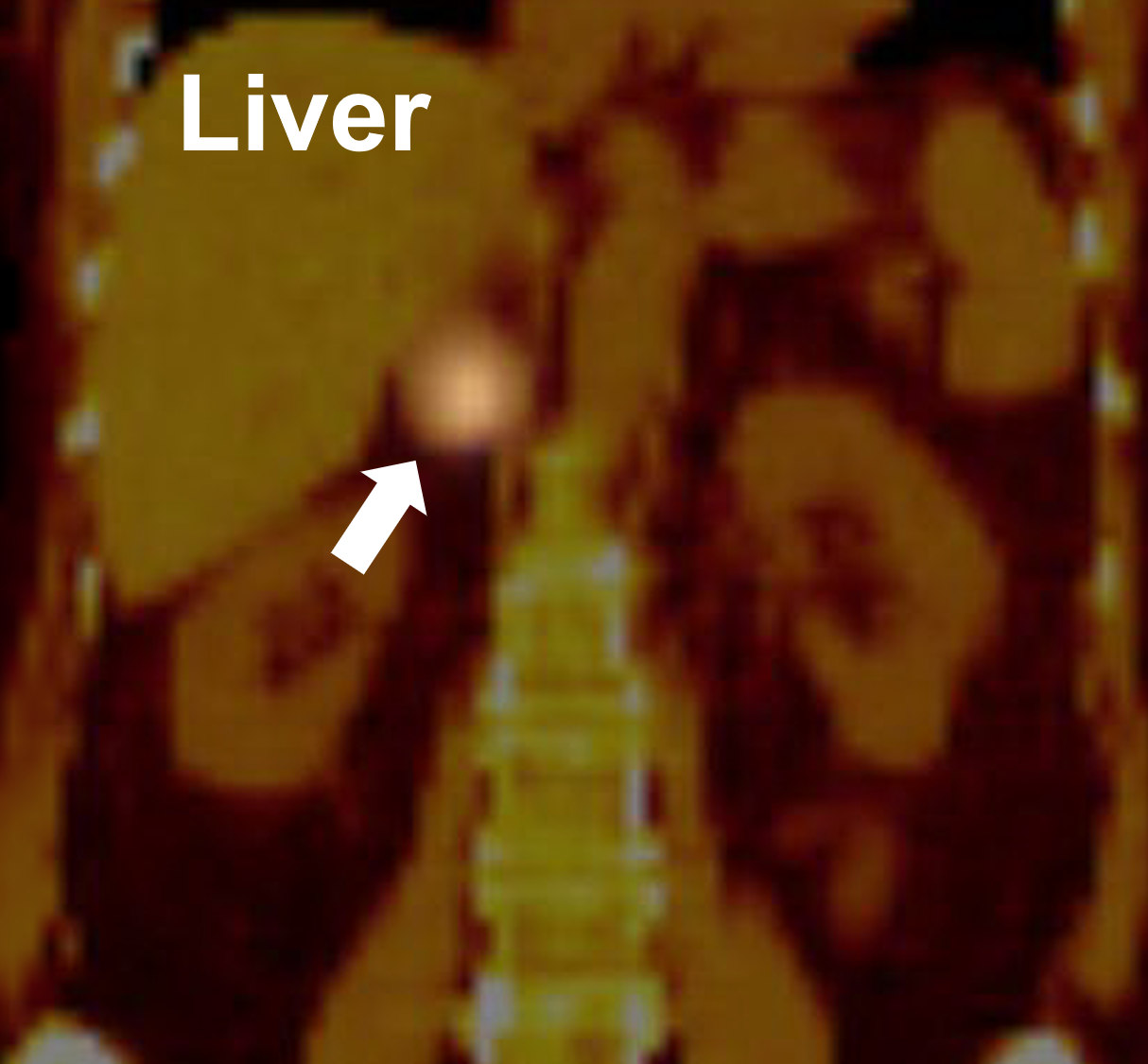
 A 68 DOTATATE PET/CT scan for malignant pheochromocytoma demonstrating multiple metastatic lesions in bone and lymph nodes (arrows).
The DOTATATE scan is a more recent technology and expression of somatostatin receptors by pheochromocytoma and paraganglioma cells facilitates targeted PET imaging with 68-Ga-DOTA-peptides. a-68 DOTATATE PET/CT detected similar number but has significantly greater lesion-to-background contrast compared to FDG PET/CT. DOTATATE PET/CT should now be considered the ideal first line investigation for imaging pheochromocytoma and paraganglioma. Depending on DOTATATE findings and the clinical question, FDG and MIBG remain useful and, in selected cases, may provide more accurate staging, disease characterization and guide treatment choices
A 68 DOTATATE PET/CT scan for malignant pheochromocytoma demonstrating multiple metastatic lesions in bone and lymph nodes (arrows).
The DOTATATE scan is a more recent technology and expression of somatostatin receptors by pheochromocytoma and paraganglioma cells facilitates targeted PET imaging with 68-Ga-DOTA-peptides. a-68 DOTATATE PET/CT detected similar number but has significantly greater lesion-to-background contrast compared to FDG PET/CT. DOTATATE PET/CT should now be considered the ideal first line investigation for imaging pheochromocytoma and paraganglioma. Depending on DOTATATE findings and the clinical question, FDG and MIBG remain useful and, in selected cases, may provide more accurate staging, disease characterization and guide treatment choices
Regular PET (18-FDG-PET/CT) is mainly used to image malignant (cancerous lesions). It is an imaging modality which is very useful in adrenocortical carcinoma and metastasis to the adrenal gland (most commonly carcinomas of the lung, breast, kidney, and melanoma). In adrenocortical cancer, 18-FDG-PET/CT can be more accurate than a CT scan and may identify metastasis (spread) for instance to lymph nodes and the liver not detected on the CT scan.
As a functional imaging modality, 18-FDG-PET/CT, which provides glucose metabolic information on malignant tumors, has shown great results for the detection of adrenal metastases. It is used in many cancer patients (including lung, breast, kidney, colorectal cancer and melanoma) and provided information for diagnosis, surveillance, and following therapy in these cases. Occasionally, an adrenal metastasis is the only evidence of cancer, and in those cases an adrenalectomy is indicted. Learn more about adrenal surgery for metastasis here.
Ultrasound to Evaluate Adrenal Tumors and Growths
Ultrasound is the fastest, cheapest, and most readily available scan to look at the kidneys and adrenal glands. But, it is the least accurate, so it is usually not used as much as the CT scan. It can be used to examine any type of adrenal tumor but it is not very good so don't bother.