Adrenal Surgery Can Be Performed 8 Different Ways Depending on the Skills and Experience of the Surgeon
Adrenal surgery can be performed eight different ways. Some are MUCH better than others, but which one you get will be determined by the experience of your surgeon, and NOT what is best for you. You must do your homework! Here we provide an overview of the 8 very different surgical techniques a surgeon can use to remove an adrenal gland or adrenal gland tumor. As you will read, some of these techniques are still commonly used, but should not be! Surgeons without much experience perform adrenal surgery in same way as they learned to perform gallbladder or hernia surgery and these techniques should not be used for adrenal surgery.It is unfortnuate that 90% of adrenal surgery is performed by surgeons who do fewer than 4 or 5 adrenal operations per year. They almost always use techniques that are outdated or not the best choice, and the patients suffer because of it. Please choose your adrenal surgeon wisely--your local general surgeon or urologist is very unlikely to be the best choice for you.
The 8 Good and Bad Techniques for Adrenal Surgery:
#1) Mini Back Scope Adrenalectomy (MBSA). Posterior Retroperitoneoscopic Adrenal Operation.
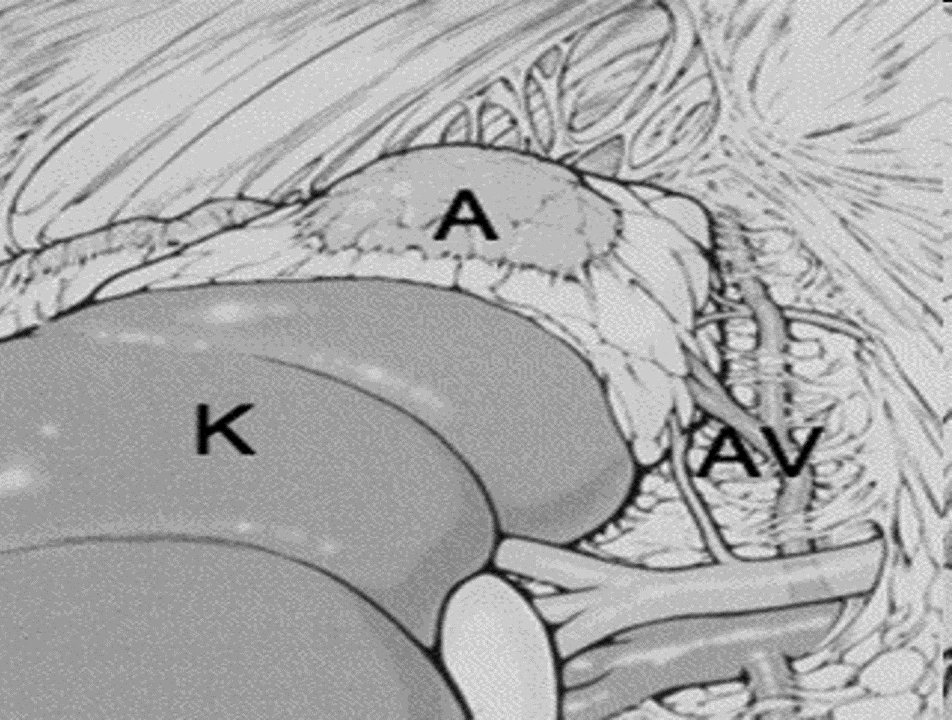 The view of the retroperitoneal space during a left Mini Back Scope Adrenalectomy (MBSA). K = kidney, A = adrenal, AV = left adrenal vein and artery.
This minimally invasive adrenal operation is performed with 1 small scope port placed through the lower part of the patient's BACK, and 2 other small instrument ports (on the sides of the lower back because the arenal glands are in the very back of the abdomen). Thus, we refer to this operation as the Mini Back Scope Adrenalectomy (MBSA).
The Mini Back Scope Adrenalectomy (MBSA) is preferable for the vast majority of adrenal tumor patients, as it uses an endoscope and very small incisions (0.5-1.1 cm; less than 1/2 inch). The Mini Back Scope Adrenalectomy (MBSA) is the preferred operation for more than 95% of patients with adrenal tumors.
Please do not have any of the other options listed below. Most people get these inferior operations because their surgeon does not know how to perform the most advanced procedures. This is the Mini Back Scope Adrenal operation that Dr. Carling performs on about 95% of his patients and usually takes him less than 25-35 minutes to complete. We have two entire pages dedicated to the Mini Back Scope Adrenalectomy (MBSA), and its benefits.
The view of the retroperitoneal space during a left Mini Back Scope Adrenalectomy (MBSA). K = kidney, A = adrenal, AV = left adrenal vein and artery.
This minimally invasive adrenal operation is performed with 1 small scope port placed through the lower part of the patient's BACK, and 2 other small instrument ports (on the sides of the lower back because the arenal glands are in the very back of the abdomen). Thus, we refer to this operation as the Mini Back Scope Adrenalectomy (MBSA).
The Mini Back Scope Adrenalectomy (MBSA) is preferable for the vast majority of adrenal tumor patients, as it uses an endoscope and very small incisions (0.5-1.1 cm; less than 1/2 inch). The Mini Back Scope Adrenalectomy (MBSA) is the preferred operation for more than 95% of patients with adrenal tumors.
Please do not have any of the other options listed below. Most people get these inferior operations because their surgeon does not know how to perform the most advanced procedures. This is the Mini Back Scope Adrenal operation that Dr. Carling performs on about 95% of his patients and usually takes him less than 25-35 minutes to complete. We have two entire pages dedicated to the Mini Back Scope Adrenalectomy (MBSA), and its benefits.
#2) Laparoscopic Trans-Abdominal Adrenalectomy (LTA). This is a laparoscopic operation (laparoscope - a long fiberoptic cable connected to a camera) that goes through the front of the abdomen. This is the adrenal operation that most surgeons with little expertise in adrenal surgery perform. It is simply a modification of the laparoscopic operation they perform for gallbladder and hernia surgery. This is NOT the best adrenal operation for 95% of people, but it is by far the most common adrenal operation performed because 90% of adrenal operations are performed by surgeons who are not experts in adrenal surgery and perform 4 or fewer (yes, four or fewer) adrenal operations per year. There are no expert adrenal surgeons who perform adrenal surgery with this method. Dr. Carling uses this method in fewer than 5% of the hundreds of adrenal surgeries he performs each year. Yet it is the most common adrenal operation because non-experts who have zero specialized training in adrenal surgery are doing most adrenal operations. You should avoid this operation and find a surgeon with more expertise.
Another unfortunate fact is that the most commonly performed adrenal operation (the laparoscopic adrenal operation that goes through the FRONT of the abdomen) is NOT the best operation for almost every patient. The best operation for almost all adrenal tumor patients is the Mini Back Scope Adrenalectomy (MBSA) through the patient's BACK.
This laparoscopic transabdominal adrenal operation does allow small to moderately-sized tumors to be removed using scopes and small incisions. This technique is tolerated well and, because it is done with scopes, the surgeons who do this operation will call it "minimally invasive adrenal surgery". Compared to the Mini Back Scope Adrenalectomy (MBSA), patients tend to have more pain after the operation, longer hospital stays and recovery time as well as slower return to work and normal activities.
Why should laparoscopic and robotic (through the belly) adrenalectomy be avoided? Read more on our adrenal surgery blog
#3) Laparoscopic Hand-Port Assisted Trans-Abdominal Adrenalectomy.
 A huge right pheochromocytoma resected by Dr. Carling via Laparoscopic Hand-Port Assisted Trans-Abdominal Adrenalectomy. On the CT scan, the white arrow delineates the 15 cm right adrenal mass. The gray arrow demonstrates an 1 cm intra-tumoral pseudoaneurysm which occasionally occurs in pheochromocytomas.
This surgical technique to adrenal tumors is a hybrid between laparoscopic transabdominal adrenalectomy (LTA) and open standard trans-abdominal adrenalectomy. The positioning of the patient and approach is similar as the laparoscopic transabdominal adrenalectomy (LTA). This approach is appropriate for larger tumors (>7-12 cm) and tumors which are suspected to be malignant, or very large, aggressive pheochromocytomas. Also, this approach may be used dependent on the patient’s body habitus (especially obesity). This is the preferred operation that the adrenal surgery experts like Dr. Carling use for patients with very large adrenal tumors. This operation is NOT the preferred method to remove small adrenal tumors which makes up about 95% of patients with adrenal masses. We have videos of Dr. Carling performing this operation.
A huge right pheochromocytoma resected by Dr. Carling via Laparoscopic Hand-Port Assisted Trans-Abdominal Adrenalectomy. On the CT scan, the white arrow delineates the 15 cm right adrenal mass. The gray arrow demonstrates an 1 cm intra-tumoral pseudoaneurysm which occasionally occurs in pheochromocytomas.
This surgical technique to adrenal tumors is a hybrid between laparoscopic transabdominal adrenalectomy (LTA) and open standard trans-abdominal adrenalectomy. The positioning of the patient and approach is similar as the laparoscopic transabdominal adrenalectomy (LTA). This approach is appropriate for larger tumors (>7-12 cm) and tumors which are suspected to be malignant, or very large, aggressive pheochromocytomas. Also, this approach may be used dependent on the patient’s body habitus (especially obesity). This is the preferred operation that the adrenal surgery experts like Dr. Carling use for patients with very large adrenal tumors. This operation is NOT the preferred method to remove small adrenal tumors which makes up about 95% of patients with adrenal masses. We have videos of Dr. Carling performing this operation.
#4) Open Standard Trans-Abdominal Adrenalectomy. In this adrenal operation, the surgeon approaches the adrenal glands through an incision on the anterior abdominal wall. Think of this as a typical, old-fashioned operation where a large incision (usually about 10 inches) is made and the surgeon moves the bowel and other organs out of the way to gain access to the kidney and adrenals.
This approach through the front of the abdomen should only be used for large adrenal tumors (>12 cm, more than 5 inches) and those adrenal massses/tumors which are suspected or known to be malingnant (cancerous), especially if the tumor is invading surrounding structures such as the kidney, liver, spleen, pancreas, bowel, or major vessels such as the inferior vena cava (IVC). Dr Carling only uses this standard trans-abdominal operation for these large, cancerous adrenal tumors. If your surgeon has planned to perform this operation and you have a small tumor (less than 3 cm) then you need to get a second opinion. This likely would only be done in this instance if your surgeon is not an expert at adrenal surgery and that is all he knows.
#5) Open Thoraco-Abdominal Adrenalectomy. This option allows the greatest exposure to the adrenal gland and all the surrounding structures and therefore is only used for the very largest adrenal tumors and masses. This technique entails making a large incision which traverses both the abdominal and thoracic (chest) cavities, including some the diaphragm that separates them. This large operation is reserved for only the largest and most malignant tumors of the adrenal gland in hopes of the providing adequate exposure of the tumor and its blood supply to allow curative resection. This approach is primarily used for large tumors (>12 cm, 5 inches) and tumors that are suspected or known to be malignant, especially if they are invading surrounding structures such as the kidney, liver, spleen, pancreas, bowel, or major vessels such as the inferior vena cava (IVC).
#6) Open Posterior Adrenalectomy. The posterior approach gains access to the adrenal gland through an incision in the back overlying the top of the kidney. This operation is now more of historical interest since the introduction of the Mini Back Scope Adrenalectomy (MBSA).
#7) Open Retroperitoneal Adrenalectomy. The retroperitoneal technique combines the advantages of the posterior approach with the greater exposure gained by the anterior trans-abdominal technique. This operation is now more of historical interest since the adoption of the Mini Back Scope Adrenalectomy (MBSA). This operation is outdated and you should not have it. There are no scopes, and you will have a large incision on your back.
#8) Robotic (Robot-Assisted) Adrenalectomy. Robot adrenal surgery uses a surgical robot to expose and remove the adrenal gland. Robotic adrenal surgery started in about 2003 but it is NOT the preferred way to remove an adrenal tumor and was abandoned by all of the experts by 2010. This approach is similar to laparoscopic trans-abdominal adrenalectomy (LTA) and the Mini Back Scope Adrenalectomy (MBSA), except that the surgeon uses a robot to run the scopes and dissecting instruments instead of using these instruments with his/her hands. Again, the difference is that the surgeon has to rely on a robotic system (robot-assisted) technique. Also, the incisions are significantly larger that with the Mini Back Scope Adrenalectomy (MBSA). The reason the surgeon would use this technique is usually due to inexperience with adrenal surgery, and not having performed enough minimally invasive adrenal operations; Mini Back Scope Adrenalectomy (MBSA). Also, robotic adrenalectomy often takes 3-5 h (5-10 times longer than Mini Back Scope Adrenalectomy; MBSA). Again, Robotic Adrenalectomy is NOT the preferred way to perform adrenal surgery and very few people benefit from this.
It is possible that robotic surgical systems in the future will become significantly better, more minimalistic, less expensive and cumbersome, without the current potential increased harm to the patient. Thus, the surgeons of the Carling Adrenal Center do not perform and do not endorse robot-assisted adrenalectomy. These operations are typically performed by general surgeons and urologists who use the robot to do other operations and they are simply adapting the robot to the adrenal operation. All of the high-volume adrenal surgery experts in the world abandoned robotic adrenal surgery over a decade ago. None of the high-volume experts perform robot adenal surgery.
What do patients worry about when it comes to adrenal gland removal? Read more on our adrenal surgery blog
What Adrenal Operation is Best for Me?
The best adrenal operation depends on the problem that needs to be fixed. Since 95% of patients with adrenal tumors have a small tumor that is not cancerous, the best adrenal operation for 95% of people is the Mini Back Scope Adrenalectomy (MBSA), also called the "Posterior Retroperitoneoscopic Adrenal Operation". There are a number of factors that an expert adrenal surgeon will consider to determine which adrenal operation will be performed on any particular patient:- The size of the tumor
- The type of adrenal tumor
- The appearance of the tumor on a CT, MRI, PET or other imaging study
- A history of previous abdominal operations
- The surgeon's experience with different operations
Please do your homework before you have adrenal surgery. Very few surgeons perform 4 or more adrenal operations per year and therefore you are very likely to have a surgeon who is inexperiencedt at this operation. You will get an operation that the surgeon simply knows how to do, and verly likely NOT the operation that is best for you. If you came this far and somebody you know needs an adrenal operation, the next pages for you to read are:
- All the benefits of the Mini Back Scope Adrenalectomy (MBSA) and why it is the best adrenal operation for 95% of people with adrenal tumors.