Is it Possible to Remove Only Part of the Adrenal Gland?
There are several circumstances where it is preferable to remove just the adrenal tumor without removing all of the normal adrenal gland with it. This is called partial adrenalectomy or, more technically, a "cortical-sparing" adrenalectomy. The goal is to leave some normal adrenal tissue behind so that we can avoid adrenal insufficiency (not enough adrenal hormones leading to the requirement to take hormone supplements). In other words, removing both adrenal glands would require the patient to take adrenal hormones and other medications every day for the rest of their life. If the surgeon can remove only part of one adrenal gland, preserving some normal adrenal cortex tissue, then the patient may not have to take any adrenal hormones or medications.
 Dr. Carling performing a bilateral cortex-sparing Mini Back Scope Adrenalectomy (MBSA) in a young patient with familial bilateral pheochromocytoma.
Of course, if the patient has two adrenal glands and the surgeon is going to remove just one, then a partial cortical-sparing adrenal operation is not necessary. The patient still has a complete normal adrenal gland on the other side--and all you really need is about one-third of one gland to live normally and not take medications every day. So this partial adrenal operation is only relevant if the patient has problems in both adrenal glands whereby they both must have some portion of a tumor removed.
Dr. Carling performing a bilateral cortex-sparing Mini Back Scope Adrenalectomy (MBSA) in a young patient with familial bilateral pheochromocytoma.
Of course, if the patient has two adrenal glands and the surgeon is going to remove just one, then a partial cortical-sparing adrenal operation is not necessary. The patient still has a complete normal adrenal gland on the other side--and all you really need is about one-third of one gland to live normally and not take medications every day. So this partial adrenal operation is only relevant if the patient has problems in both adrenal glands whereby they both must have some portion of a tumor removed.
When is a Partial Cortical-Sparing Adrenalectomy Appropriate?
For optimal results, there are four crucially important concepts the patient needs to understand about the partial, cortical-sparing adrenalectomy. The ability to perform partial (or cortical-sparing) adrenalectomy is dependent on:- What type of tumor the patient has.
- The size of the tumor, as well as its relationship to the adrenal vein, surrounding organ and other structures such as the inferior vena cava (IVC).
- Whether there is sufficient tissue available to save (the tumor is not too big and the blood supply to the remaining adrenal tissue can be preserved.
- Whether the surgeon is expert enough to know how to do this more technically challenging operation. Very few surgeons have ever performed several partial cortical-sparing adrenal operations.
What is the Purpose of Partial Cortical-Sparing Adrenal Surgery?
Partial (or cortical-sparing) adrenalectomy allows for resection of adrenal tumor(s), while preserving unaffected adrenal tissue with the goal of preventing adrenal insufficiency. This is especially important in patients affected with bilateral adrenal tumors, typically pheochromocytomas, as well as those with adrenal metastasis (cancers that started somewhere else--like the breast, lung, colon, melanoma, etc--and spread to the adrenal glands).Can a Partial Cortical-Sparing Adrenalectomy be Performed via Mini Back Scope Adrenalectomy (MBSA)?
Read more about partial adrenal surgery on our adrenal surgery blog
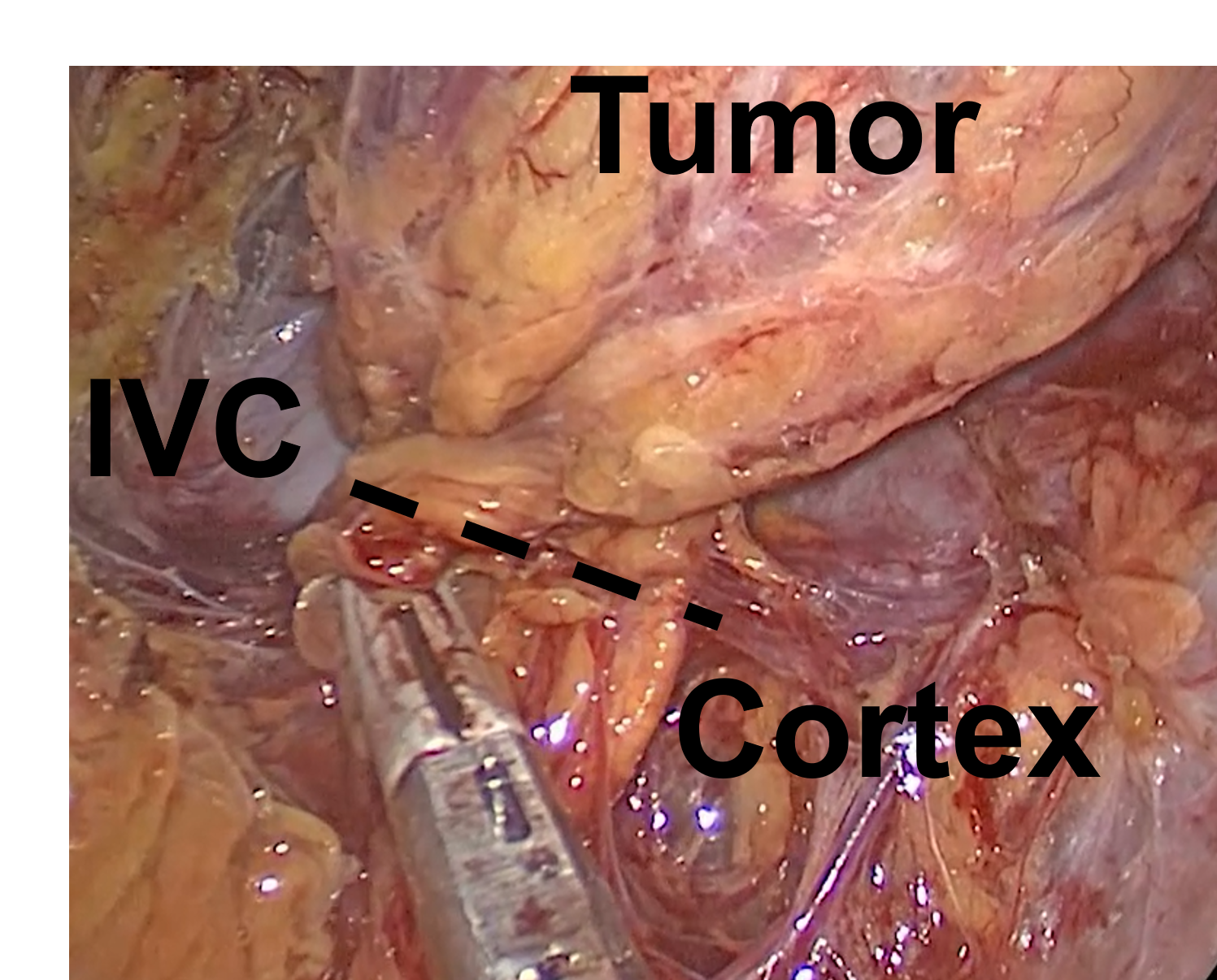 Partial Cortical-Sparing Adrenalectomy Performed via Right Mini Back Scope Adrenalectomy (MBSA). The tissue is divided at the dotted line, removing the tumor, but preserving the normal cortex and the inferior vena cava (IVC).
Absolutely! But only if your surgeon has lots of experience--most surgeons won't even attempt this. The Cortical-Sparing allows for a minimally invasive approach to adrenal gland resection compared to the more traditional laparoscopic transabdominal adrenalectomy (LTA) and open (through the abdomen) adrenal surgery. The Mini Back Scope Adrenalectomy (MBSA) technique is ideal to address patients with bilateral disease (disease in both the right and the left adrenal glands) and can be utilized in patients with, for instance, bilateral pheochromocytomas in the setting of multiple endocrine neoplasia 2A (MEN2A), von Hippel Lindau (VHL) syndrome, or in patients who have had previous adrenal surgery. We have a nice video of Dr. Carling performing a partial cortical-sparing adrenalectomy via the Mini Back Scope Adrenalectomy (MBSA) for you to watch here.
Partial Cortical-Sparing Adrenalectomy Performed via Right Mini Back Scope Adrenalectomy (MBSA). The tissue is divided at the dotted line, removing the tumor, but preserving the normal cortex and the inferior vena cava (IVC).
Absolutely! But only if your surgeon has lots of experience--most surgeons won't even attempt this. The Cortical-Sparing allows for a minimally invasive approach to adrenal gland resection compared to the more traditional laparoscopic transabdominal adrenalectomy (LTA) and open (through the abdomen) adrenal surgery. The Mini Back Scope Adrenalectomy (MBSA) technique is ideal to address patients with bilateral disease (disease in both the right and the left adrenal glands) and can be utilized in patients with, for instance, bilateral pheochromocytomas in the setting of multiple endocrine neoplasia 2A (MEN2A), von Hippel Lindau (VHL) syndrome, or in patients who have had previous adrenal surgery. We have a nice video of Dr. Carling performing a partial cortical-sparing adrenalectomy via the Mini Back Scope Adrenalectomy (MBSA) for you to watch here.
Partial (or cortical-sparing) adrenalectomy is an invaluable option for patients with genetic syndromes associated with pheochromocytomas. These syndromes include MEN2, VHL, and neurofibromatosis type 1 (NF1), as well as others. Approximately 40-80% of patients with either MEN2A or VHL will develop bilateral pheochromocytomas and these tumors are usually benign. As such, cortical-sparing adrenalectomy can remove affected tissue, while leaving behind enough tissue to prevent adrenal insufficiency with minimal risk of recurrence.
Who is a Good Candidate For a Partial Adrenal Operation?
Typically, over 90% of patients who are thought to be good candidates for partial adrenalectomy (based on preoperative imaging) will be able to undergo it. It is very important to consider the below mentioned 4 concepts to determine the ability to perform partial (or cortical-sparing) adrenalectomy:- What type of tumor the patient has.
- The size of the tumor, as well as its relationship to the adrenal vein, and other structures such as the inferior vena cava (IVC).
- Whether there is sufficient tissue available to save (the tumor is not too big, and the blood supply to the remaining adrenal tissue can be saved).
- Whether the surgeon is skilled enough to do this more technically challenging operation.
What About Patients Who Need Bilateral (both) Adrenal Glands Removed?
In cases where partial adrenalectomy is performed for bilateral adrenal tumors, >90% of patients do not require steroid supplementation (prednisone, hydrocortisone, etc). This means that >90% of patients undergoing partial bilateral adrenalectomy can be saved from developing adrenal insufficiency. In most cases with bilateral tumors, we would completely resect the entire adrenal gland on one side and then perform a partial resection on the other side. However, this has to be individualized in each scenario. The key to prevent adrenal insufficiency is to save at least 30% of one gland, or a total of 15% of both adrenal glands.Watch a video a of Dr Carling performing a partial (or cortical-sparing) adrenalectomy.