Atypical Adrenal Masses: Why Small Tumors Can Still Mean Big Cancer Risks—and What to Do About It

Atypical Adrenal Masses: Why Small Tumors Can Still Mean Big Cancer Risks—and What to Do About It
Imagine getting a routine scan for an unrelated issue, and your doctor identifies a small mass on your adrenal gland. At around 2 cm, it seems minor, and the usual advice might be to monitor it. However, a significant study in The Journal of Clinical Endocrinology & Metabolism (2025, Vol. 110, No. 7) changes that perspective. It reveals that atypical adrenal masses, even those smaller than 4 cm with unusual imaging characteristics like high density (elevated Hounsfield Units or HU on CT scans), carry a substantial risk of being cancerous.
This multicenter research, based on data from 2000 to 2020, emphasizes the importance of evaluation and, in many cases, removal. As the founder of the Carling Adrenal Center, the leading institution for adrenal surgery worldwide, I've seen how prompt action with the right technique can improve outcomes. Let's review the findings, their implications, and why surgery—particularly our Mini Back Scope Adrenalectomy (MBSA)—is often the best approach.
.jpg)
What Are Atypical Adrenal Masses?
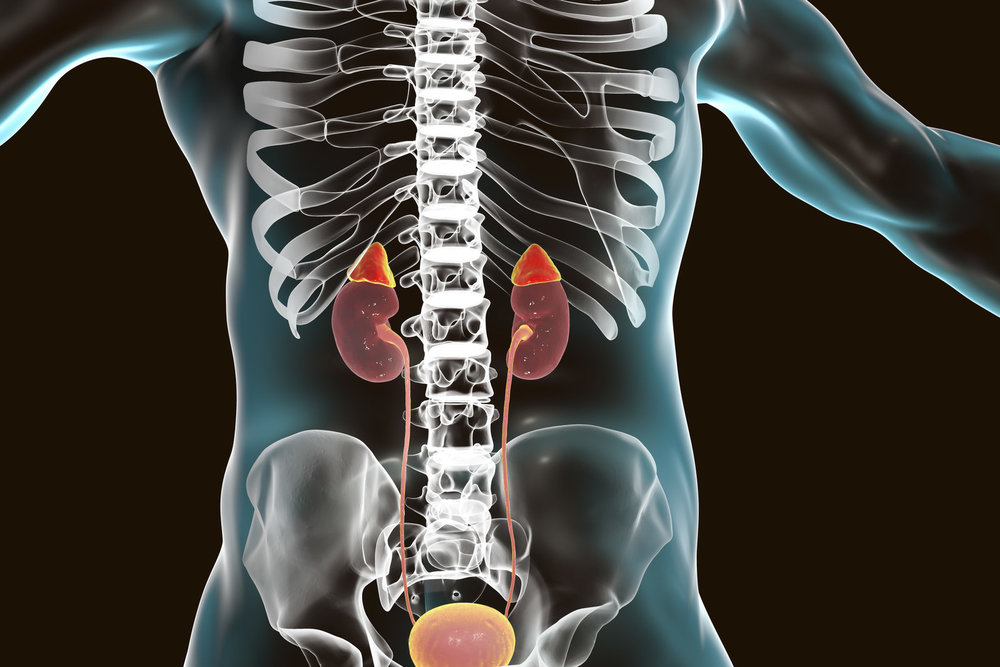
Adrenal masses are frequently discovered, affecting 5-7% of adults who undergo abdominal imaging. Most are benign adenomas, appearing as low-density lesions (<10 HU) on CT due to their lipid content. Atypical adrenal masses show higher density (>10 HU) and account for up to 30% of these discoveries. They can include pheochromocytomas (tumors that disrupt blood pressure regulation), metastases, or adrenocortical carcinomas (ACCs)—aggressive cancers that can spread if not addressed.
The study examined 217 adults over 18 with tumors at least 1 cm, followed for a minimum of 6 months. It excluded cases with prior treatments or clear non-tumors like hemorrhages. The cohort was 61.1% female, with a median age of 58; masses were typically incidental (77.7%), detected on CT (80.1%), and unilateral (98%). Pathological analysis of 71 masses—primarily from surgery —uncovered concerning patterns.
The Cancer Risk Hiding in Small Sizes
The central insight: Size alone doesn't determine safety. Traditional guidelines often suggest observation for masses under 4 cm, but these atypical ones averaged 2 cm initially, and 25 were confirmed ACCs. They demonstrated faster growth (up to 2.7 mm per year) than benign cases, comparing rates for cancers, adenomas, and observed masses.
Why You Should Care
Atypical adrenal masses represent more than incidental findings—they can lead to significant health issues. ACC is uncommon but lethal, with 5-year survival rates of 20-50% if detected early, declining further with spread. The study addresses limitations in prior research, highlighting growth trends that call for revised management strategies. Risks extend to hypertensive crises from pheochromocytomas or indicators of other underlying conditions.
For patients, these discoveries can cause concern, affecting diverse groups—unilateral masses, slightly more common on the left. The key message? Unusual imaging warrants a thorough endocrine review to prevent hormonal imbalances or malignant progression.
Time to Act: Get It Removed
Observation may suit very low-risk cases, but for atypical adrenal masses with concerning features, surgery is generally recommended. Guidelines advocate removal for suspicious lesions, and this study supports earlier intervention for high HU or growth. Biopsies are not recommended; complete evaluation provides definitive diagnosis and resolution.
Success depends on the method. Conventional robot-associated or laparoscopic surgeries (through the abdomen) involve greater recovery time and risks, such as injury to nearby organs.
The Carling Adrenal Center: Your Best Bet for Safe Removal
At the Carling Adrenal Center in Tampa, Florida, we specialize exclusively in adrenal conditions, performing more surgeries than any other facility in the world. Our Mini Back Scope Adrenalectomy (MBSA) sets the standard—this approach uses a small posterior incision for direct access, bypassing the abdomen.
Why Choose MBSA:
- Minimally Invasive: Small incisions mean less pain and minimal scarring.
- Best: The operation takes minutes as opposed to hours through the belly
- Quick Recovery: Patients often go home the same day and return to normal routines within 48 hours, not weeks.
- Reduced Risks: Complication rates below 0.2%, avoiding abdominal organ involvement.
- Proven Effectiveness: Close to 100% success in full tumor removal, well-suited for these smaller atypical masses.
At the Carling Adrenal Center, you receive comprehensive care, from pre-op hormone assessments to ongoing monitoring. We're the preferred choice for patients globally due to our consistent results.
Figure 1: Dr. Carling inspecting that the positioning of the patient is perfect prior to proceeding with Mini Back Scope Adrenalectomy (MBSA).
Steps You Can Take Right Now
If an adrenal mass is identified:
- Seek Specialized Evaluation: Consult an adrenal expert for HU analysis and hormone testing.
- Monitor Changes: If surgery is not indicated right away, then follow up with imaging in 6-12 months; rapid growth calls for action.
- Prioritize Removal: For atypical masses under 4 cm with elevated HU, opt to get it removed—MBSA offers a straightforward, effective solution.
- Manage Related Conditions: Address blood pressure or metabolic concerns that could compound issues.
- Stay Informed: Review your imaging and collaborate with a specialist team.
Moving Forward
This research study shifts the focus, advocating guidelines that prioritize imaging characteristics over size alone. While retrospective with some constraints, it opens doors to future studies on underlying mechanisms, perhaps leading to alternative treatments.
If you have an atypical adrenal mass, take control: Get it removed safely and promptly to minimize cancer risks. Contact the Carling Adrenal Center—we're ready to help you navigate this and regain your health.
Reference
The Natural History and Malignant Potential of Atypical Adrenal Masses: A Multicenter Retrospective Cohort Study. J Clin Endocrinol Metab. 2025;110(7):e2184-e2190.
Additional Resources:
- Learn more about the Carling Adrenal Center
- Learn more about Dr. Tobias Carling
- Learn more about our sister surgeons at the Norman Parathyroid Center, and Clayman Thyroid Center.
- Learn more about the Hospital for Endocrine Surgery