Frying Your Adrenal Tumor: Is That a Good Idea?

Frying Your Adrenal Tumor: Is That a Good Idea?
High blood pressure, or hypertension, is a silent epidemic, afflicting millions and straining hearts, kidneys, and brains. For about 5% of patients, the root cause is a tiny, benign tumor in the adrenal gland called an aldosterone-producing adenoma (APA). These tumors churn out excess aldosterone, a hormone that disrupts salt and water balance, spiking blood pressure. Traditionally, treatment involves invasive adrenal vein sampling (AVS) to locate the tumor and laparoscopic adrenalectomy to remove the entire gland—a process that’s effective but requires a hospital stays. A new study, FABULAS, tests another approach: endoscopic (inserted through the patient’s mouth) ultrasound-guided radiofrequency ablation (EUS-RFA), which zaps left-sided APAs through the stomach. While the effort to treat primary aldosteronism (PA) is commendable—given that less than 0.1% of PA patients are ever diagnosed or treated—the procedure’s flaws pale in comparison to the gold standard: function-preserving partial adrenalectomy, particularly via the Mini Back Scope Adrenalectomy (MBSA) at the Carling Adrenal Center.
The FABULAS study, published in The Lancet (February 2025), explored EUS-RFA across three UK hospitals from 2018 to 2023. In this trial, 28 patients underwent 35 ablations, targeting left-sided APAs with a catheter that delivers radiofrequency energy to destroy the tumor. The results showed promise: no major safety issues, such as perforation or bleeding, occurred. At three months, 75% of patients achieved complete or partial biochemical cure (normalized aldosterone levels), and 43% saw improved blood pressure. Four patients even ditched their medications entirely, with blood pressure below 135/85 mmHg. The procedure is relatively quick, scarless, and allows next-day return to normal life—whereas the MBSA is associated with some discomfort for a few days. Kudos to the FABULAS team for tackling PA, a condition so underdiagnosed that most patients languish untreated, their hypertension mislabeled as “essential” while cardiometabolic risks mount. Their innovative spirit is a beacon in a field where less than 0.1% of PA sufferers get the care they need.
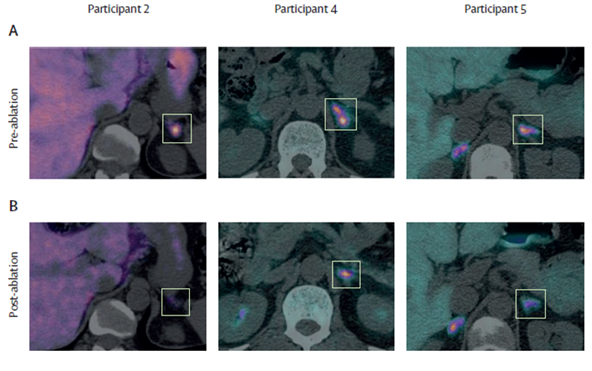
Figure: The left adrenal aldosterone-producing adenomas (APAs) before and after being burned in 3 study participants in the Lancet study out of the U.K.
But here’s the rub: EUS-RFA has serious limitations that make it a risky bet compared to the precision of function-preserving partial adrenalectomy, especially the MBSA perfected at the Carling Adrenal Center. First, ablation risks tumor spillage. Unlike surgery, which cleanly excises the tumor, RFA fragments it, potentially scattering tumor cells. These cells could implant and re-grow, leading to high recurrence rates—a nightmare that could necessitate repeat procedures or full adrenalectomy, erasing RFA’s minimally invasive edge.
Second, RFA obliterates the tumor tissue, making it impossible to perform CYP11B2 staining, the definitive test for confirming an APA’s aldosterone-producing nature. This pathology is critical not only for verifying the diagnosis but also for assessing whether the procedure achieved a biochemical cure and ruling out aldosterone overproduction from the contralateral adrenal gland. In FABULAS, pre-ablation biopsies were attempted, but six nodules lacked CYP11B2 expression, suggesting misidentification or sampling errors. Without intact tissue, clinicians are left guessing about the procedure’s success or the risk of persistent disease.
Third, EUS-RFA is only feasible for left-sided APAs. The left adrenal’s proximity to the stomach allows trans-gastric access, but the right adrenal, nestled behind the liver, is out of reach. This limits RFA to roughly half of APA patients, leaving the rest to face surgery or lifelong medication. In contrast, the MBSA, performed at the Carling Adrenal Center, is equally effective for both sides, offering a universal solution.
Fourth, FABULAS’s small sample—28 patients—leaves the procedure’s safety profile murky. The risk of thermal injury to nearby structures, like the pancreatic tail or renal vessels, remains unquantified. A misstep could trigger pancreatitis or vascular damage, complications that larger studies, like the ongoing WAVE trial, must clarify. The Carling Adrenal Center’s MBSA, by contrast, boasts a robust track record, with thousands of procedures demonstrating minimal complications and maximal gland preservation.
The MBSA at the Carling Adrenal Center is a game-changer for PA patients. Unlike traditional adrenalectomy, which removes the entire gland, MBSA targets only the tumor, preserving healthy adrenal tissue. This approach, perfected by Dr. Tobias Carling, uses a small incision and a retroperitoneoscopic technique to access the adrenal gland with unparalleled precision. The benefits are profound: patients retain adrenal function, avoiding hormone replacement; recovery is swift, often within days; and outcomes are stellar, with very high biochemical and clinical cure rates for APAs. The Carling Adrenal Center’s expertise—handling over 2,000 adrenal surgeries—sets a benchmark that EUS-RFA can’t yet touch. MBSA’s ability to preserve gland function while eliminating the tumor makes it far superior, especially for younger patients or those with bilateral disease.
Since the 1980s, there have been attempts at “frying” endocrine tumors using RFA, including parathyroid tumors causing primary hyperparathyroidism, but those attempts have not gained traction as the treatment is far inferior to surgical removal.
FABULAS’s heart is in the right place. PA is a major driver of hypertension, causing 5-13% of cases and at least 25% of treatment-resistant ones. Its cardiometabolic toll—doubling the risk of heart and kidney damage—demands action. The study’s 77% reduction in aldosterone levels and decreased reliance on antihypertensives are steps forward, especially for patients unfit for surgery. Patient surveys, including 126 from the International Primary Aldosteronism Foundation, show enthusiasm for less invasive options, even if less effective than surgery. This patient-driven push, coupled with molecular imaging advancements that spot tiny APAs (some just 12 mm), underscores the need for innovation. FABULAS deserves applause for trying where so few do—less than 0.1% of PA patients ever get diagnosed, let alone treated.
Yet, EUS-RFA’s flaws—tumor spillage, loss of diagnostic pathology, left-side limitation, and unknown thermal risks—make it a distant second to MBSA. The Carling Adrenal Center’s approach offers what PA patients need: a precise, function-preserving cure with proven results. EUS-RFA might appeal to those desperate for alternatives, but its risks and uncertainties demand caution. Larger trials may refine it, but for now, “frying” your adrenal tumor pales next to the surgical precision of MBSA. If you’re among the lucky 0.1% diagnosed with PA, head to the Carling Adrenal Center—your adrenal gland deserves better than a zap.
Reference
Argentesi G, Wu X, Ney A, Goodchild E, Laycock K, Lee YN, Senanayake R, MacFarlane J, Ng E, Kearney J, O'Toole S, Salsbury J, Carroll N, Gillett D, Tadross JA, Marker A, Godfrey EM, Goodchild G, Bestwick JP, Gurnell M, Cheow H, Pereira SP, Drake WM, Brown MJ; FABULAS study group. Endoscopic, ultrasound-guided, radiofrequency ablation of aldosterone-producing adenomas (FABULAS): a UK, multicentre, prospective, proof-of-concept trial. Lancet. 2025 Feb 22;405(10479):637-647
Additional Resources:
- Learn more about the Carling Adrenal Center
- Learn more about Dr. Tobias Carling
- Learn more about our sister surgeons at the Norman Parathyroid Center, and Clayman Thyroid Center.
- Learn more about the Hospital for Endocrine Surgery